-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Soft tissue augmentation techniques
Key points
- Take the periodontal biotype into consideration when choosing a certain soft tissue augmentation technique.
- Achieve a sufficient amount of keratinized gingiva.
- Proper abutment selection.
Gingival biotype plays an important role in determining tissue levels achieved around implants. A thin biotype is generally more susceptible to recession of the facial mucosal margin or permeation of a gray color from the implant, induced by the resorption of a thin labial cortical plate. The use of a subepithelial connective tissue grafts (SCTG) or free gingival grafts (FGG) converts a thin gingival biotype into a thick gingiva (Mathews, 2000), which can enhance the long-term gingival marginal stability and simplify tissue management during the restorative treatment procedures, improving the tissue thickness. An adequate zone of attached gingival may also be necessary around dental implants to conceal the implant collar and the abutment-restoration interface inter-proximally. In addition, they create the illusion of root prominence and increase the width of the crestal peri-implant mucosa in order to provide an emergence profile for the restoration and enable the constructed site to closely resemble a natural tooth.
Different techniques could be used to improve the amount of soft tissue simultaneously with implant placement and/or during the second stage surgery:
- Connective tissue graft (CTG) or acellular dermal matrix with a coronally advanced flap (CAF);
- Connective tissue graft acellular dermal matrix in combination with an envelope flap or pouch (tunnel technique);
- Free gingival graft;
- Pediculated connective tissue graft (PCTG):
Connective tissue graft or acellular dermal matrix with a coronally advanced flap
Connective tissue graft have been used to produce root coverage at multiple adjacent gingival recessions associated with gain in the CAL and in the width of KT, and for augmenting alveolar ridge contours. When indicated and properly utilized, these surgical procedures can provide stable and significant gains in soft tissue volume and contour that can contribute to the successful esthetic management of implant sites.
Connective tissue graft acellular dermal matrix in combination with an envelope flap or pouch
This technique optimizes vascularity by eliminating the need for vertical releasing incisions. Furthermore, when adjacent recession defects are present and are connected by an esthetically critical papilla, this technique is an excellent approach to protect the positional height of the papilla. This flap design, in combination with partial-thickness dissection, creates the most optimal and vascular sub-gingival environment for the placement of subepithelial or acellular collagen matrix type of grafts.
Free gingival graft
The use of autogenous FGG in mucogingival surgeries are considered a reliable and efficacious approach for augmenting peri-implant soft tissue defects and are most often utilized to increase the amount of keratinized tissue around an implant.
Pedunculated connective tissue graft
Among the techniques used in the management of peri-implant tissue, the papillae regeneration technique by Patrick Palacci helps in recreating reliable and reproducible tissue formations similar to pre-existing interdental papillae.
Figure 1 Figure 2
Figure 3 Figure 4
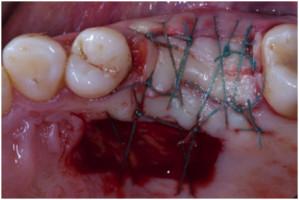
Figures 1-4: connective tissue graft with a coronally advanced flap
Figure 5 Figure 6 Figure 7 Figures 5-7: connective tissue graft with a coronally advanced flap
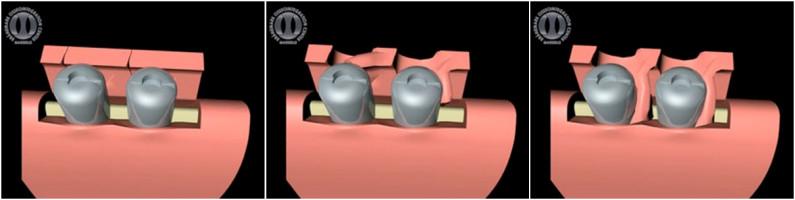
Figure 8: Palacci’s flap
Figure 9 Figure 10 Figure 11 Figures 9-11: Free gingival graft