-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Screw-retained restorations, esthetic zone
Key points
- Ideal implant placement to achieve screw retention in the anterior zone is critical.
- The choice to screw retain final restorations have a definitive advantage.
- There are multiple abutment options to facilitate screw retention.
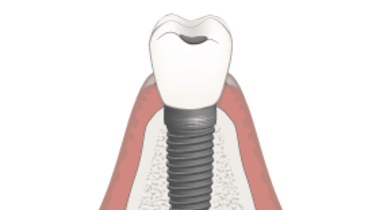
Esthetic implant restorations in the anterior zone depend on precise implant placement. Understanding the relationship of the implant to adjacent structures (implant / tooth) to preserve the inter-proximal bone, to the buccal plate, and the depth at which the implant is placed related to the osseous base will result in a predictable outcome. (Tarnow et al.)
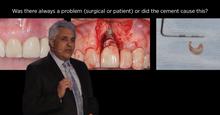
The biological advantages of using screw retention and eliminating a luting have been addressed in the current literature. There is evidence that the presence of cement not completely removed acts as medium for bacterial colonization contributing to late implant failure due to progressive bone loss.
In order to place implants in a ideal position it is recommended that a surgical guide be utilized, after the diagnostic wax phase, to aid in the implant placement. The value of three dimensional imaging cannot be underestimated in the maxillary anterior to visualize buccal plate.
Once the implant has been placed (depending on the implant) there are multiple abutment options. If the lingual access is achieved with the placement of the implant, a stock / or custom abutment / or restoration directly to the implant with a single crown can be considered.
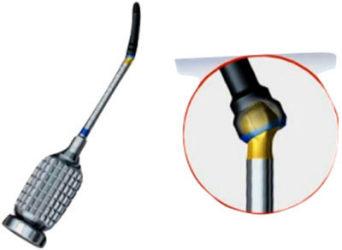
With the introduction of the angulated screw channel (ASC) available with the Nobel Active implant and the new NobelReplace Conical connection, the access to the implant abutment screw can be accessed with as much as a 25 degree deviation from the long axis. With the Nobel Tri-lobe connection or an external hexconnection implant axis deviation of the abutment can be corrected with stock custom angulated abutments in varying degrees. If the stock option does not satisfy the esthetic requirements a custom abutment can be fabricated and a set screw can be tapped into the abutment thus retaining the crown from a lingual access position.
Finally the material for the abutment can be fabricated from either metal or ceramic depending on the specific implant system and esthetic requirements for the patient.
Figure 1: Angulated Screw Channel showing metal adapter to implant Figure 2: Omnigrip driver (left) and Omnigrip Screw (right) for Angulated Screw Channel Figure 3: All ceramic abutment prepared for porcelain application and final screw retained restoration
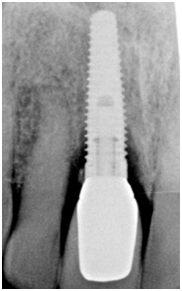
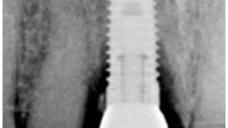
Figure 4: #7 (12 Int) and #10 (22 Int) restored with screw retained implant full crowns Figure 5: #7 (12 Int) direct to the implant Figure 6: #10 (22 Int) with custom abutment and lingual set screw
Figure 7: #8 ( 11 Int) implant full crown screw retained. Figure 8: Radiographic evidence of cement resulting in bone loss