-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Cement-retained restorations, esthetic zone
Key points
- The practitioner may chose to cement retain the final restoration.
- The choice cement final restorations mirrors conventional prosthodontics.
- There are multiple abutment choices for cement retention.
- The practitioner must decide to use a provisional or permanently cement the restoration.
Esthetic implant restorations in the anterior zone depend on precise implant placement. Understanding the relationship of the implant to adjacent structures (implant / tooth) to preserve the inter-proximal bone, to the buccal plate, and the depth at which the implant is placed related to the osseous base will result in a predictable result. (Tarnow et al. and other articles)
In order to place implants in a ideal position it is recommended that a surgical guide be utilized, after the diagnostic wax phase, and digital treatment planning with NobelClinician software. This serves as an invaluable aid for restorative-driven implant placement. The value of three dimensional imaging cannot be underestimated in the maxillary anterior to visualize buccal plate, interproximal bone, and circumferential height of bone and the position of the final restoration.
Once the implant has been placed (depending on the implant) there are multiple abutment options. If the lingual access is achieved with the placement of the implant, a stock or custom abutment is considered. The stock abutments can be made of titanium, zirconia, or other metal compositions. These can be placed directly in on the implant and prepared with copious amounts of water to achieve the ideal marginal form, and preparation characteristics for ideal retention and resistance form. A provisional is then fabricated, placed and the soft tissue contours developed and allowed to mature prior to final impressions. These abutments can also be prepared in the dental laboratory, with the provisional and placed, thus avoiding intra oral preparation.
With the advent of CAD/CAM a custom abutment of ideal geometry and form can be fabricated. The literature is conclusive that these abutments have at least equal accuracy of fit to the implant surface with the advantage of being able to use a wide choice of materials (Zirconia, Titanium, Gold, Metal ceramic alloys etc) Thus all machining is done precisely and the abutment is “clean” of any residual materials that may cause soft tissue irritation.
The final choice for the practitioner is choice of cement. First the whether to use a provisional or permanent cement. The ability to gain access to the abutment screw cannot be over emphasized. Even with following all the manufactures recommendations and achieving the desired torque values, screws come loose. This complication is easily dealt with if the restoration can be removed, the screw tightened and the restoration salvaged. If one uses a permanent luting agent the restoration will need to be destroyed to reach the abutment screw in most instances.
The choices of permanent luting agents are diverse, with resin cements becoming more popular due to their superior characteristics while being insoluble. These cements are also available in a variety of shades to optimize esthetics depending on the material choice for the final restoration.
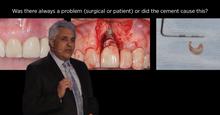
There is evidence that the presence of cement not completely removed acts as medium for bacterial colonization contributing to late implant failure due to progressive bone loss. Since some of the resin cements are not radiopaque and may extrude along the implant surface. It is strongly recommended that a meticulous cementing procedure be followed.