-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Single tooth efficiency model (STEM)
Key points
- Local conditions; patient in need of single-tooth extraction because of trauma/fracture, external/internal root resorption, advanced caries/periodontal disease.
- Consider patient´s general/local symptoms, clinical and radiographic signs of infection, condition of adjacent teeth, patient´s desires/expectations.
- Extraction resulting in intact alveolar bone walls, elimination of infection, and provided that standard prerequisites are at hand for implant placement, consider STEM, i.e. extraction with immediate implant placement and immediate loading.
Assessments/Diagnostics
Special attention should be paid on oral hygiene, health condition of adjacent teeth (active caries lesions, former restorative treatment, periodontal status) and other oral tissues (remaining alveolar bone volume, pathology within alveolar bone, mucosa condition).
What are the expectations from the patient?
Consider age of the patient and the best timing to perform the procedure. A majority of trauma cases are adolescents, not fully grown up and not with stable occlusion. Decide treatment strategies prior to permanent treatment.
Treatment considerations/procedures
Provided that standard requirements for single implant treatment are fulfilled, i.e. sufficient alveolar bone dimensions, any infection present may be eliminated during the procedure, adjacent teeth in good condition, completed growth of the jaw, etc, STEM may be suggested. STEM implies facilitated and faster treatment with one surgery only:
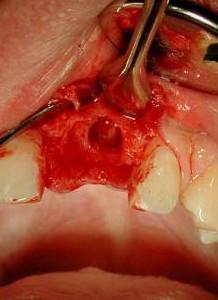
- Extraction aims at jaw bone preservation (Figures 1-5)
- Careful inspection of alveolus, eliminate granulation tissue as sign of infection
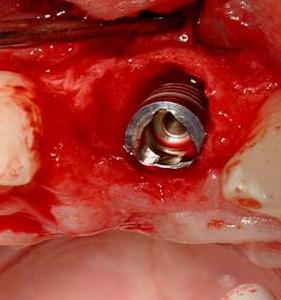
- Extend site preparation apically of alveolus for primary implant stability
- Aim at implant insertion torque ≥30 Ncm or resonance frequency value ≥ 60 ISQ (implant stability quotient) for one-stage surgery
- Fill any gap between implant periphery and bone wall of the alveolus (Figures 6,7). Autogenous bone /bovine particles/bone substitute materials may be used
- Connect abutment and wound closure. Deliver a provisional crown, adjusted out of occlusion (Figures 8-11)

Figure 1
Figure 2 Figure 3 Figure 4
Figures 1-4: Tooth 21 (#9 UNIV) presenting with external/internal root resorption (arrow). Careful extraction with periotome instrument, aiming for bone preservation.
Figure 5 Figure 6 Figure 7 Figure 8
Figures 5-8: Intact bone walls, immediate implant placement, discrepancy between former root size and implant diameter, abutment placed to receive immediate provisional crown
Figure 9 Figure 10 Figure 11
Figures 9-11: After extraction of tooth 41 (#25 UNIV), placement of implant/abutment and an immediate provisional crown (out of occlusion)