-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Suture removal
Key points
- Typically, sutures would be ideally removed 8-12 days after placement.
- Resorbable sutures offer the advantage that they may not be removed.
- Suture removal is usually a quick and pain free procedures, and there is no need for anesthetic.
Sutures are available in a number of types and sizes (diameter) to ensure that wound margins are free of tension, allowing healing by primary intention. Dental sutures are classified into two types, absorbable and non-absorbable. They can also be classified as mono-filament or multi-filament, based on their construction, and whether they are made from natural or synthetic materials.
Suture removal depends on the material and procedure. Generally, the healing of the wound takes place after 8 to 12 days. At the start of the process, the patient might feels a firm tug on each stitch if they end up dragging knotted end through the healing tissue. Nevertheless, anesthetic is usually not needed.
Abandoning a suture submucosally can lead to foreign body reactions, infection and eventually implant loss.
Even resorbable sutures may benefit from removal of remnants after healing. The suture should be clearly identified, then pulled towards the wound with a hemostat or cotton forceps and taken out using a scissors or a blade. After removal of sutures it may be good to swab the mucosa clean from any debris with moist gauze.
In case of major surgical procedures or in patients suffering from bleeding disorders, it is preferably remove first one out of two sutures to verify that the wound closure holds. Otherwise the rest of suture removal is postponed.
After suture removal, the patient will continue the specific oral hygiene procedures pre-scribed after surgery for 2-3 days.
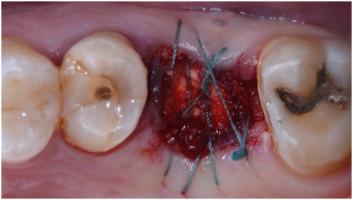
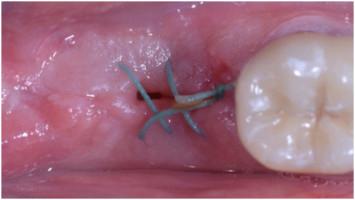
Figure 1: Extraction Figure 2: Suture removal 12 days after surgery.
Figure 3: Extraction Figure 4: Suture removal 12 days after surgery Figure 5: 3 weeks follow-up