-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Sinus lifting
Key points
- Grafting of the maxillary sinus is the most commonly used and a very predictable procedure for vertical bone augmentation in the posterior segment of the edentulous maxilla
- Sinus floor augmentation is either performed by an external or an internal (transcrestal) approach
- Sinus floor augmentation can be performed with immediate or delayed implant placement (in terms of primary implant stability)
- Bone substitute materials are as effective as autogenous bone for sinus floor augmentation.
Indications
Less than 4-6 mm of vertical residual bone height in the posterior segment of the maxilla is an indication for a sinus augmentation procedure [Esposito].
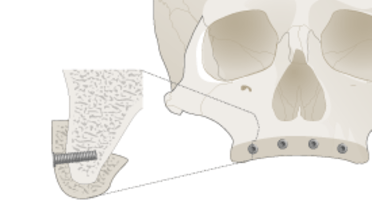
External approach
The external access to the maxillary sinus is carried out at a lateral buccal alveolar aspect, the Schneiderian membrane is elevated and the resulting space filled with a bone graft or bone substitute [Esposito, Schmitt]. Implants can be placed immediately with sinus augmentation or delayed. An advantage of the external approach is the good overview. Whether the external window needs to be covered by a membrane is currently under debate.
Internal approach
The internal approach is carried out through the implant bed. After initial drilling the Schneiderian membrane is elevated transcrestally, i.e. with osteotomes and the resulting space is filled with a bone graft or bone substitute. This is followed by implant placement. Significantly more vertical bone height can be gained with a lateral sinuslift approach [Esposito 2010].
Treatment protocol
Implants are either placed simultaneously with sinusgrafting (one-stage approach) or after a healing period of 4-8 months following sinusgrafting (two-stage approach) [Esposito, Schmitt]. This is dependent on primary implant stability. The limit of residual vertical bone for a one-stage approach is stated as 4 mm in the literature [Esposito].
Bone substitutes
Multiple bone substitute materials and/or autologous bone grafts can be used for sinuslifting [Schmitt]. In terms of implant survival and newly formed bone, bone substitutes are comparable to particulated autologous bone [Schmitt]. Some even reached a successful outcome without placing a bone substitute [Pinchasov 2014].
Complications
The most common complication is the perforation of the Schneiderian membrane. This can occur during access preparation and/or elevation of the membrane [Esposito 2010]. Small perforations can be covered with a resorbable collagen membrane and the grafting procedure can be completed. In terms of an extensive perforation, surgery has to be terminated and grafting cannot be performed. One should at least wait 6 months before retrying.