-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Need for grafting
Key points
- Reduced bone volume or unfavorable shape of alveolar bone may require grafting or bone augmentation prior to implant placement
- Depending on shape of bone defect lateral or vertical graft procedures are applied
- For a better diagnosis 3-D computed tomography is preferrable
Indication for grafting - Anatomical
There are three main indications for grafting from an anatomical perspective:
- Vertical bone deficiency
- Horizontal bone deficiency
- Local bone defect
Indication for grafting - Clinical
From a clinical perspective, two additional considerations are important factors when considering the need for grafting:
- Inadequate bone volume for reliable implant insertion
- Excessive risk of intra- or postoperative mandibular fracture
Is grafting necessary?
In a patient-centered approach, avoiding bone grafting must be considered when alternative options offer a predictable outcome: use of less/short/narrow implants, use of zygomatic anchorage.
To ensure the correct diagnosis and need for grafting, 3-D CT images should preferrably be available. Some examples of grafting need and process include:
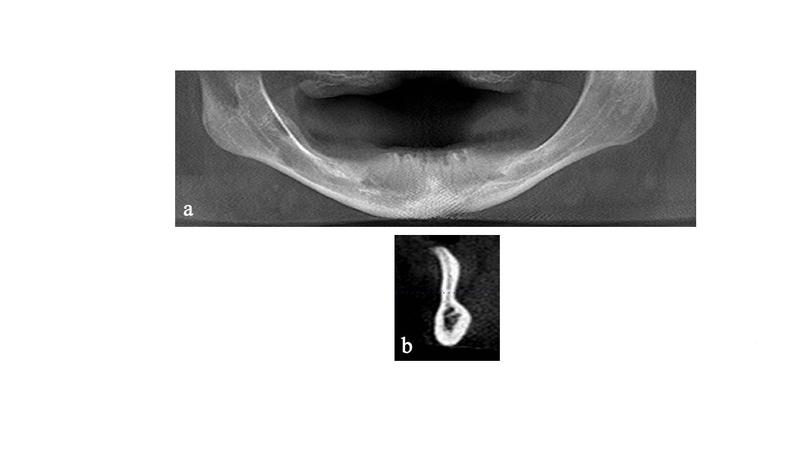
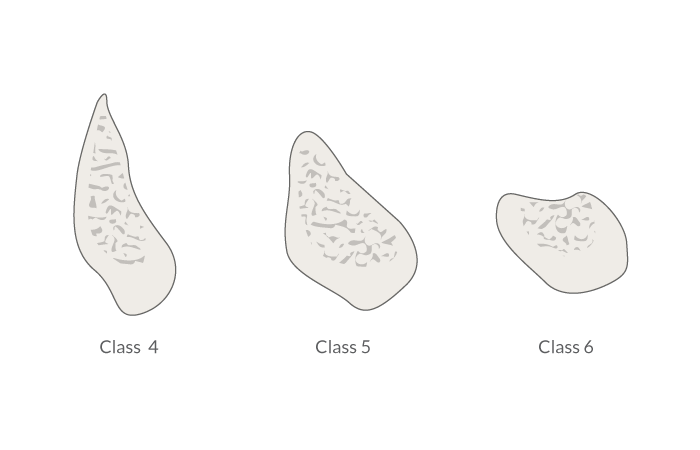
- Lateral grafting in case of Cawood class 4 with a marked knife-edge ridge of the alveolar process (Fig 1 & Fig 2).
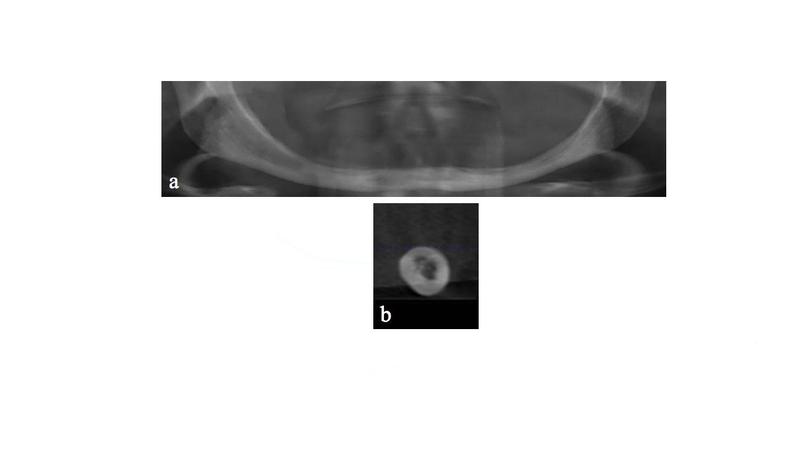
- No grafting necessary in case of Cawood class 5 (Fig 1). Insertion of implants without grafting is feasible.
- Vertical grafting in case of Cawood class 6 with complete absence of the alveolar process and extreme atrophy of the mandibular body (Fig 1 & 3). In such cases a height of the mandible of >7 mm and of the horizontal width of >6 mm is considered a clinical indication for grafting.
- Vertical grafting is indicated in case of extensive local bone defects.
Clinical topics
Questions
Ask a question
Log in or sign up to continue
You have reached the limit of content accessible without log in or this content requires log in. Log in or sign up now to get unlimited access to all FOR online resources.
No payments necessary - FOR is completely free of charge.