-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Post operative soft tissue management
Key points
- The postoperative soft tissue management can coincide with the regular control recalls
- Evaluate wound healing, and manage any signs of inflammation or infection
- Adapt provisional denture to soft tissue situation meticulously
Post operative soft tissue management - Timing
After treatment of edentulous patients, there is no need to schedule specific recalls for soft tissue control. Traditional post-operative controls at day 1 - 3, day 7 - 14 and week 4 - 6 after surgery involve soft tissue control and management.
Assessment of soft tissue during recall visits
Check condition of wound closure and sutures. In case of wound dehiscency re-suture and/or if needed place additional sutures (only within 24 to 48 hours).
Examine for signs of inflammation and infection such as swelling, exudate, pain, bleeding
Assess plaque accumulation and oral hygiene. Remove plaque when present and reinstruct oral hygiene when needed.
Advise rinsing two to three times per day with an antiseptic mouth rinse such as 0.2 % Chlorhexidine, starting the day after surgery.
Reassess at the 2nd post-operative recall at day 7 -14.
Soft tissue and provisional denture fit
Control meticulously the fit of the provisional denture to avoid tissue trauma. Since soft tissues change during the healing, adapt the denture accordingly with a soft relining when necessary.
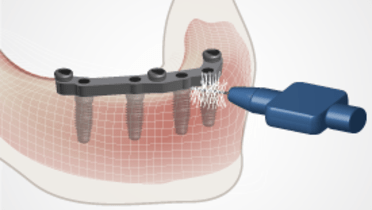
Check if bars and abutments are designed correctly and are not causing tissue hyperplasia.
If a suture granuloma occurs, and if abundant tissue is developing, remove the hyperplastic tissue, with a soft tissue laser, electrocauter or scalpel. A soft tissue laser provides usually good results, with limited bleeding. Also, it allows to uncover implants which are overgrown by soft tissue.
If a fistula occures after implant placement uncover the implant and fix an abutment.