-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Soft tissue and hard tissue
Key points
- If patient is wearing overdenture(s), remove them at nighttime
- Fibromae and ulcers can be caused by misfitting prostheses
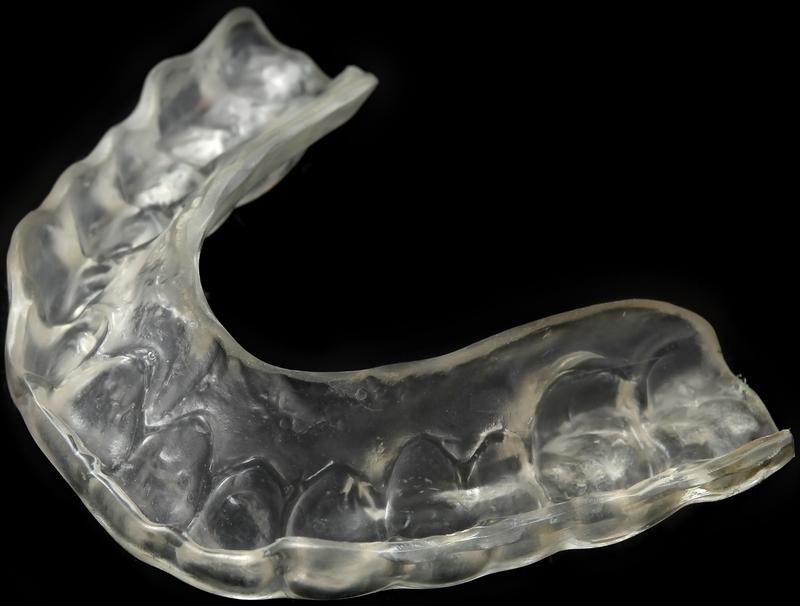
- In bruxers, a nightguard is needed when a fixed full bridge opposes the natural dentition
Soft tissue complications under removable prosthetic constructions
Removable prostheses should always be removed over night. Since the acrylic denture base is tightly covering the keratinised mucosa, it often leads to fungal/candida infections of the ginigiva under the prosthesis. The attached mucosa is presenting as red, swollen and sometimes even bleeding.
Application of miconazol gel for 1 week - twice a day, combined with the removal of the denture over night, results mostly in fast and complete healing.
Other problems include irritation fibromae or traumatic ulcers caused by misfitting prostheses. Adapting the denture provides immediate relief and cure over time. If the irritation fibroma is causing overgrowth over the attachments (ball/locator/bar), a gingival correction is needed.
Soft tissue complications underneath fixed prosthetic constructions
Due to the esthetic endeavors of the dentist or the patient demands, the space between the bridge and the gums is regularly obstructed, whereas in the past, abutments were often completely visible. Proper cleaning around the transmucosal part of the implants becomes therefore quite impossible, leading to food impaction and infections. Halitosis can also occur.
Hard tissue complications in opposite dentate jaws
Patients who are only edentulous in one jaw still have to take care of their natural dentition in the antagonist jaw. Especially the periodontal condition of the remaining teeth is of importance since we know that bacteria can translocate from periodontal pockets to formerly pristine implant/abutment surfaces. Regular dental/periodontal ccheck remains necessary. In particular the oral hygiene in the dentate jaw should be optimal.
The occlusion should be checked carefully, especially if bruxism occurs in situations where a fixed full bridge opposes natural teeth. In the latter case a nightguard has to be fabricated.