-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
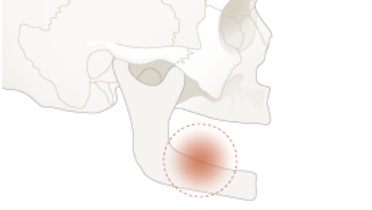
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Biologic complications
Key points
- Peri-implant mucositis appears frequently (60%) but is reversible
- A small percentage of patients develop ongoing/intermittent marginal bone loss which may have multiple causes
- Implant removal (revision surgery) is sometimes inevitable
- Patients with a history of periodontitis have a higher risk to peri-implantitis
Peri-implant mucositis
This is the reversible inflammatory process in the soft tissues around functioning implants.
Peri-implant mucositis occurs in almost 60% of subjects (± 30% of sites), restored with implants.
Diagnosis is stated by clinical examination: redness, edema, hyperplasia, bleeding on probing and sensitivity on probing, may occur at the infected implant site(s). Pus discharge is a strong diagnostic sign. Recessions are not always detectable, radiological bone loss is generally not (yet) observed.
Main causes for peri-implant mucositis are subgingival cement remnants and/or a lack of compliance to oral hygiene and maintenance. The restoration/suprastructure design and accessibility of the peri-implant tissues for cleaning can play a role and interfere.
Therapy consists of removal of subgingival irritation factors and both professional plaque removal besides reinstruction of proper home care. This will reverse the infection completely.

Peri-implantitis
This is the inflammatory process of soft and hard tissues surrounding the implant, leading to marginal bone resorption, and eventually to implant loss. There is no consensus on the threshold of marginal bone loss to define presence of periimplantitis.
Peri-implantitis occurs, but depending a lot on its definition, in 20% of subjects (± 10% of sites) restored with oral implants. Peri-implantitis, an ill-defined entity has variable threshold levels in literature and has many etiologies which should be identified during aftercare encounters in order to ensure an adequate treatment. Possible etiologies reach from subgingival cement remnants to occlusal overload and from surgical bone trauma at implant insertion to untreated prolonged perimucositis. Too often, because of the similarity with the term periodontitis, periimplantitis is a common denominator for any infection of the periimplant tissues. It is not enough to deal with the infection and inflammation. An etiologic treatment should be instituted.
Marginal bone loss of ≥2 mm compared to initial radiographs (at suprastructure installation or within the first 3 months) associated with bleeding on probing should lead to further examinations, including repeated radiographs to confirm or invalidate the suspicion of peri-implantitis.
The diagnosis is based on suppuration, deepening of the pockets around the implant and progressive marginal bone loss. Smoking, untreated periodontitis in the opposite jaw, former peri-implant mucositis and inadequate oral hygiene are regular causes of the infection. Only repeated standardized radiographs using a parallelling technique allow for a correct determination of marginal bone loss.
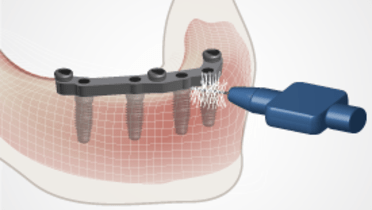
Different treatment strategies are suggested: only 1-2% of implant patients effectively need peri-implantitis surgery. For the decontamination of the infected implant surface, rinsing with saline, cleaning with cotton pellets with saline, mechanical debridement, Er:YAG laser treatment all seem equally efficient. Implantoplasty through open flap surgery can also be performed.
When advanced marginal bone loss is observed, even revision surgery with replacement of the implant should be considered.