-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Intraoral radiographs
Key points
- The intraoral technique provides mesio-distal (horizontal) and crestal-apical (vertical) measurements, as well as useful information on bone structure and density.
- Additional computerized advantages include the ability to enhance the image for viewing.
- The paralleling technique should always be attempted before other techniques.
Intraoral radiographs still remain one of the most important imaging modalities available in dentistry to the dental practitioner. The intraoral technique provides high spatial resolution imaging of teeth and potential associated dental and jawbone diseases. With careful attention to calibration and with meticulous technique for detector positioning, intraoral radiographs yield the essential diagnostic information for dental implant planning. In addition to mesio-distal (horizontal) and crestal-apical (vertical) measurements, they provide useful information on bone structure and density.
A full-mouth intraoral series include14 to 21 radiographs and it is most often done during first visit or follow-ups. Intraoral periapical radiographs can also provide a baseline standard against which subsequent radiographs can be compared to monitor changes over time. Marginal bone height around implants is considered one of the most important method for monitoring peri-implant bone health, and it is still used as a measure of implant success.
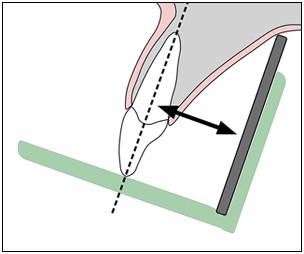
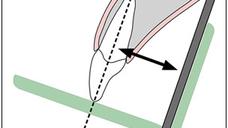
Two types of exposure techniques may be used for intraoral periapical radiography: the paralleling and the bisecting angle technique (Figures 1 and 2). With the paralleling technique, the tooth and the sensor are both kept on a parallel planes. This technique provides less image distortion and reduces excess radiation to the patient.
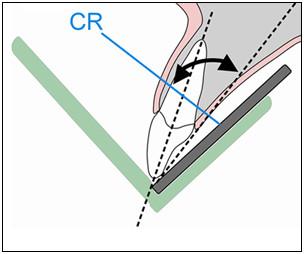
The bisecting angle technique is accomplished by placing the receptor as close to the tooth as possible. The central ray of the x-ray beam should be directed perpendicular to an imaginary line that bisects or divides the angle formed by the long axis of the tooth and the plane of the receptor. This technique is used in areas where the parallel technique is impossible due to poor access, making the angle between tooth and film more than 15 degrees.
The paralleling technique should always be attempted before other techniques. When the alveolar crest is considerably atrophic, a small size of detector should be used to reduce the risk of distortion.
As technology advances, digital detectors are gaining in popularity since they are considered part of optimization to reduce the radiation dose, maintaining high image quality. Additional computerized advantages include the ability to enhance the image for viewing.
Figure 1: Paralleling technique Figure 2: Bisecting angle technique
Figure 3: Pre extraction Figure 4: Pre implant Figure 5: 1 year








About X-ray dental intraoral
Hello!If you can help me with something. Should the room where X-ray dental intraoral is located be isolated with Pb to work with it, or it can be used in normal dental ordinance without isolation?
Hello!
If you can help me with something. Should the room where X-ray dental intraoral is located be isolated with Pb to work with it, or it can be used in normal dental ordinance without isolation?