-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Submerged vs non-submerged
Key points
- Minimal inflammation and movement of implants are critical to osseointegration.
- A non-submerged implant placement may imply early loading, shorter treatment period, and less patient morbidity with one surgical procedure only.
- Poor primary implant stability implies a submerged implant placement.
Oral endosseous implants are successful even long-term in the single-tooth situation. At insertion the primary implant stability is obtained by mechanical fixation. The secondary implant stability will result from osseointegration, a process characterized by the development of an intimate bone contact with the implant surface. The direct anchoring of bone to the implant predicts the clinical success of the implant. Inflammation of periimplant tissues and/or movement of the implant impair the osseointegration process. To minimize the risk of impaired osseointegration historically it has been recommended to insert the implant into the bone (submerged implant) and to allow for submerged healing of 3-6 months in the lower and upper jaw, respectively. After that time, during a second surgery, the implants are uncovered.
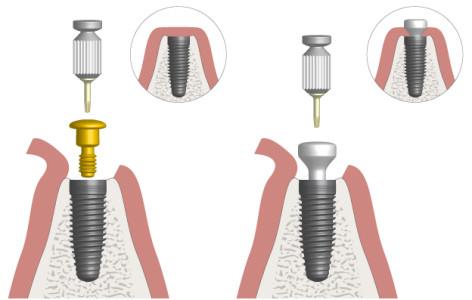
Figure 1: The principle of submerged (left) and non-submerged (right) implant insertion
Subsequent clinical studies have shown that the use of non-submerged implants reached similar long-term success as submerged ones.
Non-Submerged Implants
The treatment concept of non-submerged implant placement enables the possibility of early implant loading, one surgical procedure only, and thus a reduced treatment period for the patients. In the single-tooth case, a non-submerged implant/healing abutment may be protected from premature occlusal preload by adjacent teeth.
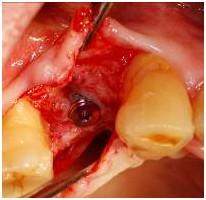
Figures 2-5: Placement of implant and healing abutment in lower right second bicuspid region according to the non-submerged concept
Submerged Implants
Submerged implant placement is still advocated in conditions of compromised bone quality, which does not allow a sufficient primary stability at insertion.
Figures 6-8: Placement of implant and cover screw in upper right first bicuspid region according to the submerged concept
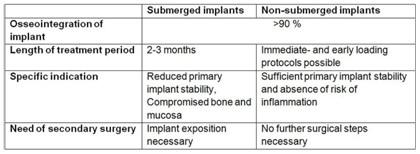
Table 1: Clinical differences between the submerged vs. non-submerged implant insertion protocol.