-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Problems and complications in maxillary implant surgery
Key points
- Complications below can occur in the maxilla regarding implant placement or bone grafting:
- Lack of primary implant stability
- Placement of the implant tip in the maxillary sinus or nasal cavity
- Perforation of the Schneiderian membrane during sinus floor elevation
- Dislocation of implants or augmentation material
- Bleeding
Complications
In the edentulous upper jaw the proximity of adjacent anatomical structures and bone density of residual bone can compromise implant insertion and may lead to complications such as lacking primary implant stability, perforation, dislocation of implants or augmentation material and bleedings.
Primary stability
Due to the bone quality of the maxilla (predominantly spongious bone) implants may lack primary stability and can loosen after insertion.
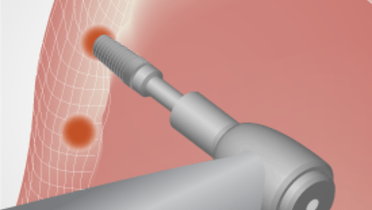
Penetration and perforation
Penetration of the maxillary sinus or the nasal cavity during implant bed preparation is a minor problem if there is adequate residual bone height for implant placement and implant primary stability. The tip of the implant should not be inserted deeper than 2 mm into the maxillary sinus.
Dislocation
Displacement of the augmentation material into the sinus happens due to perforation of the Schneiderian membrane during mobilisation and augmentation procedures of the maxillary sinus [Katranji 2008].
Implants can be dislocated into the maxillary sinus. The persistence of the implant/augmentation material in the sinus can lead to acute or chronic infections of the maxillary sinus. Dislocated implants and/ or augmentation material should be removed via a transoral or a transnasal access. Prior to the surgical intervention a 3D radiography, such as computed tomography (CT) or cone beam computed tomography (CBCT) is recommended [Sgaramella 2014].
Bleeding
An anastomosing vessel is located at the facial antral wall between the posterior superior alveolar artery and the infraorbital artery. Bleedings may occur during sinus lifting procedures. With the increase of the width of the lateral sinus wall, the vessel diameter increases as well leading to an increased risk of bleedings during surgery. The mean distance to the inferior border of the vessel from the sinus floor and from the alveolar crest can vary from 8-17 mm, respectively. Treatment of intraoperative bleedings includes: pressure, bone wax, burnish with bur and electro-cautery [Kang 2013].