-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Grafting, mandible
Key points
- Bone in the anterior region of the atrophic edentulous mandible presenting less than 5-6 mm in height and 6 mm in width requires a bone augmentation procedure for implant placement
- Autologous bone blocks are used for grafting
- Tension-free soft tissue coverage of the augmented region is mandatory to ensure sufficient wound healing and integration of the bone graft
- After grafting, alterations of soft and hard tissues must be considered and soft tissue improvements i.e. vestibuloplasty is often indicated
Indications
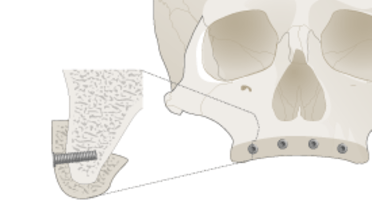
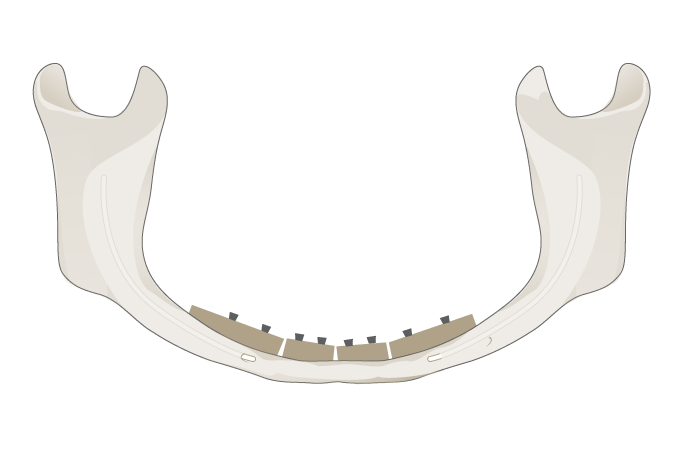
In the edentulous lower jaw implant insertion can be limited due to bone resorption processes and the resulting superficial alveolar nerve topography. In the anterior region less than 5-6 mm in height and 6 mm in width requires bone grafting before implant placement. In the posterior region an augmentation procedure is needed in cases with < 2-3 mm residual bone over the course of the alveolar nerve, but only if an implant is being considered.
Materials and techniques
Autologous bone block grafting (Fig 1) is the treatment of choice with sufficient form stability, osteoinductivity and osteogenetic properties. For harvesting big monocortical block grafts the suitable donor region is the anterior or posterior iliac crest. After bone grafting, tension-free soft tissue adaption and closure is mandatory to guarantee graft integration and to avoid wound dehiscences and infections. This leads to a shallow vestibule and soft tissue improvements, i.e. a vestibuloplasty is often indicated in the context of implant exposure.
The outcome using alternative substitutes for bone augmentations other than autologous block grafts in this indication is unpredictable and the use is not recommended due to their lacking mechanical properties and biological activity. Especially particulated bone substitutes lacking form stability are not suitable for three-dimensional augmentation. Due to the defect configuration (critical size defects lacking space) of the atrophic edentulous lower jaw stable grafts are recommended. Bone block substitutes with osteoconductive properties alone have an unsatisfactory regeneration potential for these defects.
Alternatives
For implant placement in the anterior and posterior atrophic mandible short implants, i.e. 6 mm or less are an alternative option if enough residual bone is present. Course of the alveolar nerve in the posterior segment must always be considered.
Angulated interforaminal implants are an additional option for load distribution to the posterior aspect and can avoid an augmentation procedure.