-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
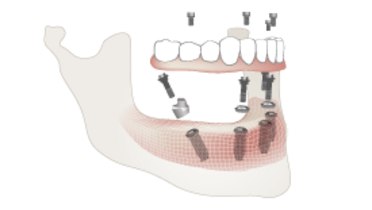
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
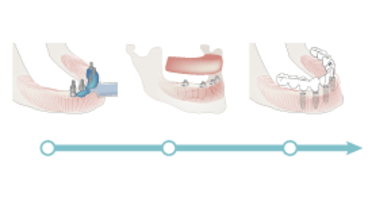
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Placement
Key points
- The prosthesis should be connected to ensuring proper seating
- Esthetics and occlusion should be carefully evaluated before torquing of retaining screws
- Post-surgical and oral hygiene instructions should be provided to the patient
Placement of provisional fixed prosthesis
Placement of a provisional prosthesis takes place by attaching the conversion denture (either patient's exisiting prosthesis or a new conversion denture) to the implants or to implant abutments. The provisional prosthesis can be attached preliminarily using temporary cylinders, one placed on each implant. Cylinders can be made from metal or plastic. Plastic cylinders are tooth-colored and are beneficial in esthetic areas whereas metal cylinders are more durable.
The conversion prosthesis is adjusted and hollowed out to permit proper seating of the prosthesis over the temporary cylinders. The cylinders may need to be shortened to permit full closure and evaluation of seating and occlusion. Autopolymerizing acrylic resin or flowable composite resin serves to fix the prosthesis to the temporary cylinders. When possible, fixation should occur with the patient in occlusion.
However, when both arches are being treated concurrently, it is advisable to seat and attach the maxillary prosthesis first and to use esthetic guidance for positioning of the occlusal plane. The mandibular prosthesis can then be attached with the patient in occlusion against the already-attached maxillary prosthesis.
Alternatively, based on an impression, the provisional prosthesis including the temporary cylinders can be fabricated in the dental laboratory.
Once attached, prostheses should be retrieved and polished after additional resin is added to fill in any voids and to attain a smooth transition between the denture base and the temporary copings. Care is taken to allow sufficient space between the intaglio surface and the soft tissue for easy access and cleaning.
The fixed prosthesis is placed and final evaluation is performed prior to tightening the screws. The abutment screws are torqued to the recommended value. Final refinement of the occlusion is performed if needed and the access holes are sealed provisionally for easy access during the upcoming phases to fabricate a definitive prosthesis.
The patient is shown how to maintain and clean the prosthesis using appropriate brushes to access the intaglio and cameo surfaces adequately. Recall appointments to evaluate healing, esthetics, function and patient comfort are scheduled.
Placement of definitive fixed prosthesis
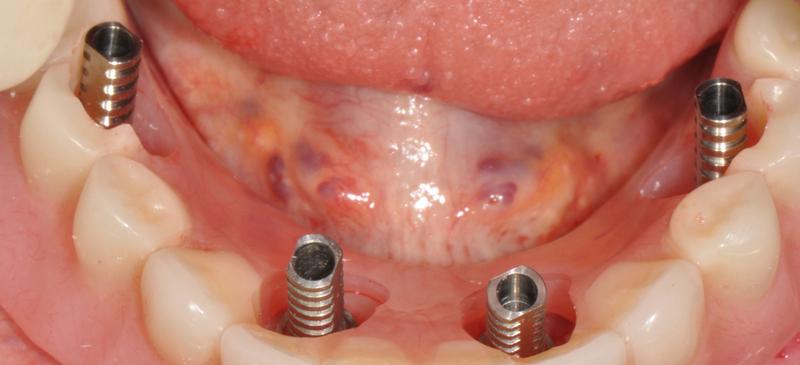
Definitive prosthesis placement takes place by attaching the prosthesis to the implants or to implant abutments. Typically, prosthesis fit is not an issue at this stage as a confirming framework try-in appointmen has taken place. Therefore, healing caps or the provisional prosthesis are removed and the definitive prosthesis attached and framework fit re-verified.
A careful evaluation of esthetic appearance, phonetic capability, patient comfort and occlusion are made and adjustments made as needed. If final polishing is needed, the prosthesis may need to be retrieved, polished and then re-placed. The abutment or retaining screws are torqued to the recommended value. Final refinement of the occlusion is performed again if needed and access holes are sealed with a resilient material over the screw head and covered by tooth or pink colored resin.
A thorough discussion between clinician and patient is necessary to calibrate patient expectations first presented during the treatment planning phase. The patient should be given clear and reasonable expectations in order to prevent dissatisfaction. In addition, the patient is shown how to maintain and clean the prosthesis using appropriate brushes to access the intaglio and cameo surfaces adequately. Recall appointments to evaluate healing, esthetics, function and patient comfort are scheduled.
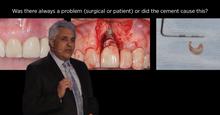
In case of cement-retained restoration designs, to avoid risk of peri-implant infammation, make sure to meticulously remove any subgingival excess cement.