-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Primary splinting
Key points
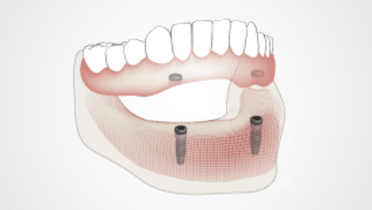
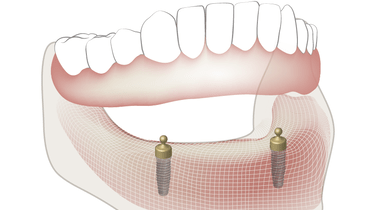
- Primary splinting refers to a direct connection of implants by means of a bar attachment
- Bar constructions provide higher retentive forces than single abutments and require less maintenance efforts
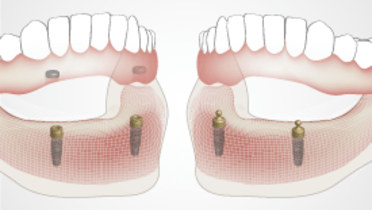
- Extension bars on 4 implants show best stability and patient acceptance
- Bar constructions require more hygiene efforts and show a higher incidence of mucositis and gingival hyperplasia compared to single abutments
Indication and principle considerations
Implant supported overdentures are an evidence-based treatment option for edentulous patients leading to a significantly increased quality of life.
There are various retention elements available which connect the implants directly (primary splinting) or which are used as single attachment on the implants (ball abutment, locators). In the latter case the implant overdenture, when seated, provides the stabilizing connection between the implants (secondary splinting). Literature data reports that the retentive attachment type does not seem to influence implant success/survival or failure rates. However, in comparison to fixed implant restorations, the implant overdenture requires higher maintenance, e.g. regarding activation or replacement of the retentive elements or the need for relining.
Advantages, disadvantages and restrictions
Bar constructions show higher retentive forces in comparison to ball or locator attachments, and especially in the case of flat posterior ridges they provide better transversal support and stability of the prosthesis. Even though the retentive elements need to be activated or replaced from time to time, according to literature data, bar constructions require less maintenance and effort in comparison to single attachments.
However, bars are more difficult to clean for the patient. Literature data reports a significantly higher plaque accumulation mainly on the mucosal surface, subsequently resulting in a higher incidence of mucositis and gingival hyperplasia.
Bar construction designs require a minimum inter-implant distance of 10-12 mm to enable positioning of the retentive attachment element. Implants positioned too far distally lead to the bar transversing the floor of the mouth and subsequently to food impaction and inconveniences for tongue movement.
The form and number of bars define the biomechanical conditions. The easiest version of a bar construction is the round bar design between two implants. In this design the bar forms a rotation axis for the prosthesis, causing posterior jaw bone resorption implying the need for regular relining of the prosthesis.
Increasing the number of implants increases the number of bar elements and retentive attachments involved in the prosthetic construction. This increased number of retention elements leads to a reduced need for activation of the retentions. Bars on 4 implants can be designed as extension bars. In analogy to fixed partial denture designs, it is recommended to place the posterior implants as distally as possible to increase the anterior-posterior spread and maximize the extensions. Comparative studies show that patients predominantly prefer extension bar constructions. Patients restored with an extension bar design report higher stability, stronger retention, improved chewing comfort and higher overall satisfaction with the restoration. Consequently a treatment plan with 4 implants can be considered the preferred treatment option.

Material selection
Bars can be fabricated with traditional casting techniques with precious and non-precious alloy selection, or with high precision CAD/CAM procedures, in titanium or Cr-Co base metal options. With casting techniques the required precision for a passive fit is difficult to achieve. Therefore modern CAD/CAM milled bars are the treatment of choice, providing multiple design options, high precision of fit and material quality, reducing laboratory effort and offering the possibility to integrate the bar design and production in a complete digital workflow.