-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Osteoporosis
Key points
- Osteoporosis is a systemic disease, affecting nearly 30% of postmenopausal women, characterized by reduced bone density and impaired microarchitecture leading to bone fractures
- Osteoporosis affects the jaw bone less than the extracranial skeleton
- Reflecting current data the success of implant surgery in osteoporotic patients is not limited
- Although antiresorptive medication is highly prescribed in osteoporosis a low risk of the antiresorptive medication related osteonecrosis of the jaw (ARONJ) exists, reflecting the low total dose over time application of antiresorptive medication in osteoporosis
Osteoporosis
Osteoporosis is a frequent disease affecting predominantly postmenopausal women. The prevalence is 7% in women aged 55 and raises to 19% in women aged 80. Osteoporosis is diagnosed by a decreased radiologic bone density (DXA-score). Primary osteoporosis is more common and is due to age-related hormonal changes, whereas secondary osteoporosis results from the presence of underlying diseases such as diabetes, corticosteroid treatment. The clinical course of both forms is characterized by fractures and their consequences. The most common treatment is the administration of antiresorptive drugs (Bisphosphonates or Denosumab).
Specific aspects of osteoporosis in jaw bone and implant surgery
Osteoporosis is a significant risk factor when surgical procedures are performed in the extracranial skeleton. This fact resembles a challenge in implant surgery procedures. However, implant surgery in the jaw bone seems not to be affected by osteoporotic bone changes. The radiologic scores of osteoporosis (DXA-score) do not correlate between extracranial skeleton and jaw bone. The use of panoramic x-ray indices for the assessment of osteoporosis in the jaw bone is limited since the BMD significantly differs between different anatomic regions within the jaw bone. Recent data (meta-analysis of clinical data) did not find a significantly increased risk of oral implant failure in osteoporotic patients.
Treatment of osteoporosis and implant surgery
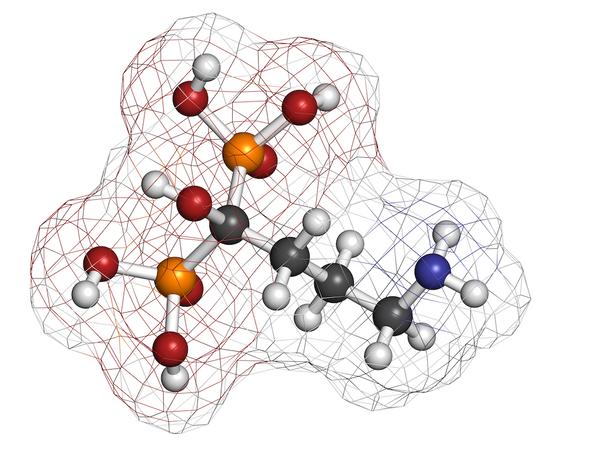
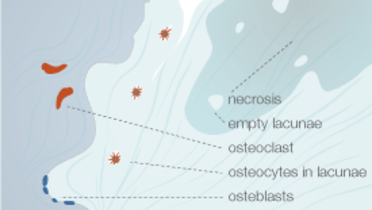
Antiresorptive medication related ostonecrosis of the jaw (ARONJ) can be triggered by oral surgical procedures carried out in patients with antiresorptive medication, used in osteoporosis treatment. The term ARONJ (Antiresorptive drug Related OsteoNecrosis of the Jaw) presently replaces the term BRONJ (Bisphosphonate Related OsteoNecrosis of the Jaw).
In contrast to patients with malignant diseases, the risk of developing osteonecrosis as a result of antiresorptive therapy in osteoporotic patients is low, due to the lower total dose and the lower frequency of application. The success rates for implants placed in these patients appear to be not different from the success rates for implants placed in patients without a history of antiresorptive treatment. Discontinuing antiresorptive medication prior to implant surgery was not shown to lower the risk of osteonecrosis but increased the frequency of skeletal related events (SRE) (osteoporotic fractures).