-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
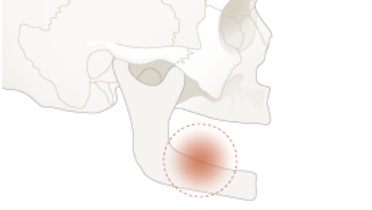
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Probing
Key points
- Probing does not cause permanent damage to periimplant tissue seal
- Connective tissue level measured by probing correlates well with underlying marginal bone height in healthy sites
- Probing depths increasing over time, associated with bleeding and eventually exudate, are a cause for concern
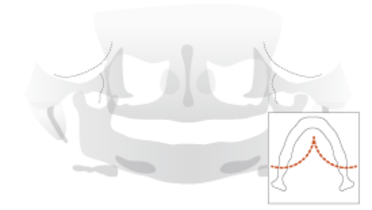
Monitoring peri-implant tissue condition
Radiographical check-ups to evaluate bone levels cannot be repeated too often to avoid unnecessary radiation. Monitoring the overlying soft tissues may help to identify eventual problems of the underlying bone, although the correlation of probing depth with crestal bone height falls as a site exhibits more soft tissue inflammation. Nevertheless, progressive increases in probing depth should lead to radiographic assessment to ascertain crestal bone height and any changes from previous viewed heights.
Probing parameters
Probing disrupts the epithelial attachment to implant surfaces but does not cause permanent damage to the periimplant soft tissue seal. Mucosal penetration around endosseous implants is similar, but not identical, to penetration of periodontal tissues. Compared to teeth, the probe tip approximates crestal bone more closely and within 1-1.5 mm The extent of probe penetration is influenced be the probing force, ideally 0.25 Newtons. Therefore, automated controlled-force probes offer better reproducibility of probing depth. Other factors that influece probing depth are angulation, probe tip diameter, implant surface characteristics, presence of cement remnants, and degree of soft tissue inflammation. Using (flexible) plastic probes prevents scratching the abutment and prosthetic surfaces, which would favor plaque accumulation.
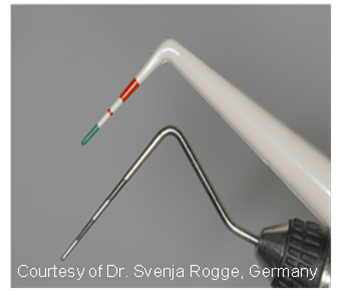
It is important to establish probing depths at the time of prosthesis placement to allow for comparison over time. A recommended method is to identify a fixed reference point on the prosthesis and measure probing depth relative to this point. However, occasionally, the prosthesis inhibits access and compromises angulation necessitating removal of the prosthesis.