-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Guided protocol, overview
Key points
- Digital workflows allow full integration of therapeutic steps from patient diagnostics and treatment planning to surgery and prosthetic design.
- Fully automated NobelClinician SmartFusion technology combines CBCT data with the model & wax-up, into a single surgical and esthetic view.
- Flapless guided surgery allows for less post-operative pain and swelling.
Digital Treatment Planning
Treatment planning involving implant placement has changed from a surgical approach, that strictly focused on bone availability, to a prosthetically driven planning using 3D imaging and computer guided software. New technologies combining data from CBCT with information on the soft tissues and crown morphology, obtained by means of optical digital high resolution scanners, allow full integration of therapeutic steps from patient diagnostics and treatment planning to surgery and prosthetic design.
For instance, NobelClinician Software (Nobel Biocare, AG), combines data from the CBCT patient scan of the model & wax-up using the NobelProcera 2G scanner (Nobel Biocare, AG) into a single surgical and esthetic view. Fully automated NobelClinician SmartFusion technology greatly simplifies the overall treatment workflow by providing an enhanced fit of the surgical guide to the patient. The clinician can take great advantage of this technology. The SmartFusion technique provides the clinician with additional information on the soft tissues.
Guided Surgery
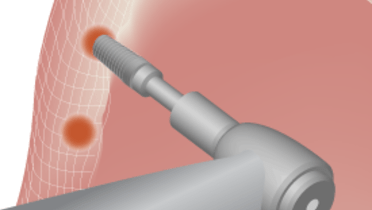
After approval, the planning may be transferred to surgery, by means of a computer aided design/computer aided manufactured (CAD/CAM) surgical template with metallic sleeves to guide the surgeon to place implants in the virtually planned position. In these cases, the surgical template is fabricated from the SmartFusion scan of the model. Implant sites are prepared according to the manufacturer’s guidelines using specially designed tools using either a fully guided surgery or a pilot drill approach.
Before surgery, the accuracy of the surgical template is checked on the master cast used for the scan. Stability of the surgical template is then tested in the patient mouth. Optionally, one to three ancor pins may be used to ensure the template stability. The surgeon may chose to use either a flapless or a flap approach. After the surgical template is removed, implant insertion torque are measured (Torque wrench, Nobel Biocare) to avoid bias due to possible attrition of the implant component on the template.
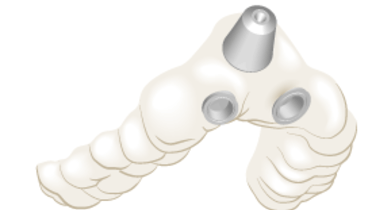
Figure 1: Optical scan of model Figure 2: Optical scan of model and wax-up Figure 3: Virtual surgical template

Figure 4: Surgical template tested on the master cast before surgery
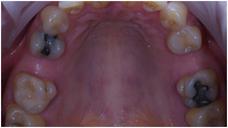
Figure 5: Intraoral view before surgery Figure 6: Implant placement thought the surgical template Figure 7: Intraoral view immediately after surgery