-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Intraoral imaging and scanning
Key points
- Digital technologies aid dentists to ensure patients receive up-to-date solutions for oral rehabilitation.
- CAD/CAM technology gives the opportunities to introduce materials that cannot manipulated by traditional techniques.
- CAD/CAM and CBCT technologies can work together through the smart fusion technology.
- CAD/CAM technology gives the opportunities to introduce materials that cannot manipulated by traditional techniques.
Digital technologies for general, cosmetic, and implant dentists, have increased significantly in the last years, allowing the patients to receive modern solutions to traditional dental problems. Digital technologies also improve communications with patients, dental technicians, and other dental specialists, enhancing diagnosis and accuracy of the treatment. Among the digital technologies available for dentistry are diagnostic imaging, intraoral imaging and scanning, including CAD/CAM restorations.
Intraoral cameras (IO cameras) produce accurate images of teeth and the supporting structures, allowing patients to see problems with their teeth and/or gums including tarnished or corroded fillings, fractured teeth etc. This also improves the communication with patient who can then better understand the need for the recommended treatment. One of the most important uses of the IO camera is by dental hygienists for educating patients about periodontal disease. It has an impact on a patient to see areas of his or her mouth that are healthy, in contrast to diseased sites.
Intraoral Optical Scanners are used in dentistry to create a digital impression of the tooth's anatomy and implant’s tridimensional position. Digital impressions offer patients the convenience of not having to endure traditional impressions: unpleasant tasting materials, bulky, cumbersome trays and possible gagging. Digital color maps can be created to provide an accurate color analysis for determining the shade and custom characterizations of cosmetic restorations.
CAD/CAM technology (computer assisted design/computer assisted manufacture) enables the production of a wide range of dental restorations, such as crowns, veneers, bridges, and implant frameworks, using a digital intuitive workflow that simulates the manual process. With an in-office computerized milling technology is possible to complete same-day tooth restorations. Alternatively, (e.g more extensive cases), it is possible to work with a dental laboratory that uses CAD/CAM technology to create final restorations. The introduction of CAD/CAM technology to manufacture dental restorations has also generated opportunities to introduce materials that cannot manipulated by traditional techniques.
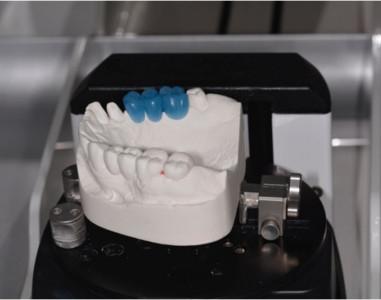
Figure 1: Optically scanning the model and waxup Figure 2: Optically scanning model and soft tissue profiles (waxup removed)
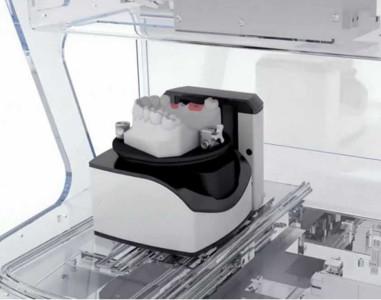
Digital technologies continue to aid dentists' efforts to ensure patients receive the best possible treatment under the most comfortable of circumstances. With a strong focus on patient safety and treatment efficiency for dental professionals and their patients, CAD/CAM technology and guided surgery using CBCT or CT scans can work together. Starting with diagnostics and treatment planning in the guided surgery software, the surface model can be obtained from a CAD/CAM scanner and can be added to the DICOM data at any stage of the treatment through a fully automated and precise smart fusion technology. This enables even better representation of intraoral tissues for diagnostics and planning. Furthermore, it reduces procedural treatment costs and shortens timelines by allowing CBCT scans to be taken at the first patient visit, offering clinicians a truly flexible way of working. Radiographic guides, specific markers and scan protocols can be avoided for partially edentulous cases. The decision for guided surgery can be taken at any stage. Fully automated, precision-fitting surgical templates are automatically generated at the click of a button using the integrated surface scan and planned implant positions.
Figure 3: Abutment designed on CAD software Figure 4: Completed, milled abutment
Figure 5: Crown Figure 6: Abutment and crown in-place