-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Cone Beam Computer Tomography (CBCT)
Key points
- CBCT provides cross-sectional imaging and 3D reconstructions of craniofacial anatomy at high spatial resolution and low radiation dose compared to spiral CT scan.
- CBCT imaging has been recommended by the American Academy of Oral and Maxillofacial Radiology as the preferred method for pre-surgical assessment of dental implant sites.
- CBCT does not provide accurate measurements of the bone density, even if a conversion ratio can be applied to provide Hounsfield Unit.
Background
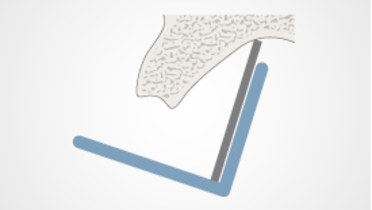
Cone beam computed tomography (CBCT) is a medical imaging technique consisting of X-ray computed tomography (CT) where the X-rays are divergent, forming a cone.
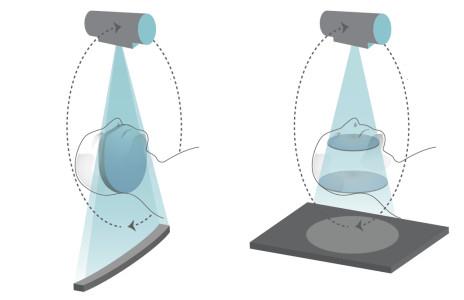
Figure 1: Comparison between CT (left) and CBCT (right) technologies.
CBCT scanners were developed in dentistry in the late 1990s, since the CBCT has become increasingly important in diagnosis and treatment planning in implant dentistry, providing cross-sectional imaging and three-dimensional (3D) reconstructions of craniofacial anatomy. In the last 10 years, CBCT has become an alternative to CT for imaging in the head and neck region, producing higher spatial resolution images at considerable lower radiation dose. The affordability of CBCT devices compared to conventional CT equipment, makes CBCT devices available in many dental clinics.
CBCT has achieved a transition of dental imaging from 2D to 3D images, overcoming limitations such as magnification, distortion, superimposition and misrepresentation of structures. The main limitation of CBCT scanners is the presence of a smaller field of view than CT because the x-ray source creates a cone-shaped beam, which rotates around a point of interest in the patient’s head as 2D image sensor intensifier plates pick up the images. In addition, Hounsfield unit measurements not as reliable as on spiral CT, even if a conversion ratio can be applied to provide Hounsfield Unit.
CBCT images have been shown to be successful for various clinical uses, including oral and maxillofacial surgery, orthodontic and endodontic therapies (Small FOVs), and implant planning and placement.
CBCT technology may be used by general dentists and specialists to improve diagnosis and treatment planning in the following cases:
- Location of anatomic structures: mandibular canal, submandibular fossa, incisive canal, maxillary sinus.
- Size and shape of ridge, quantity and quality of bone.
- Number and 3D orientation of implants.
- Length and diameter of planned implants.
- Need for bone graft, sinus lift.
- Use of implant planning software.
Digital Treatment Planning
CBCT is used for dental implant planning, specifically to measure the shape of the alveolar bone, the quality and the quantity of bone, the height and width of the planned implant site, the number, orientation of implants, the distance between the alveolar bone crest and the mandibular canal or the maxillary sinus and we can also use implant planning software. Since 2008 CBCT imaging has been recommended by the American Academy of Oral and Maxillofacial Radiology as the preferred method for pre-surgical assessment of dental implant sites.
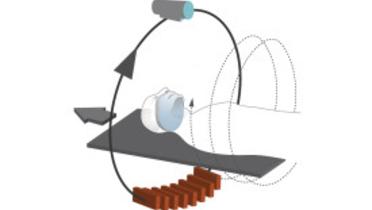
Guided Surgery
In addition, CBCT used in conjunction with third-party proprietary implant software programs allows for diagnosis and planning of the dental implant treatment. Three dimensional planning and guided surgery allow the practitioner to better diagnose and understand the extent of dental disease and to optimize virtual treatment planning. The use of an integrated treatment workflow leads to less invasive patient treatment protocols that result in high patient comfort.
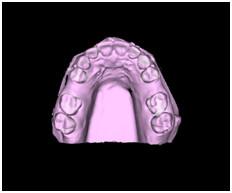
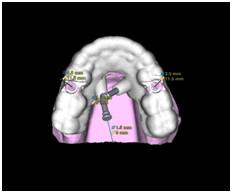
Figures 2-5: single teeth restorations planning on NobelClinician software
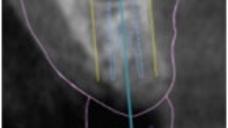
Figures 6 & 7: Guided implant placement
Figures 8 & 9: Periapical radiographs after implant placement