-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Bone volume and interdental space
Key points
- Consider available jaw bone volume in transversal (mesio-distal) and vertical dimensions using conventional intraoral radiographs. Sagittal (buccolingual) bone dimension is preferably evaluated with cross-sectional imaging.
- Base treatment options on available bone dimensions.
- Beware of root anatomy of adjacent teeth.
Bone volume/interdental space
Residual bone volume in a single-tooth gap is mainly reflected by the cause of the missing tooth. A preserved gap due to aplasia implies an under-developed alveolar crest, mainly in bucco-lingual dimension, whereas defects after extraction of compromised teeth may involve all bone dimensions. Residual bone volumes in upper lateral incisor and lower central/lateral incisor regions frequently present with transversal dimension of 5-6 mm and sagittal dimension of <4 mm, respectively.
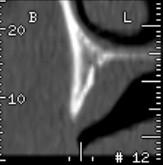
Figure 1: Insufficient sagittal bone dimension in upper lateral incisor region

Figure 2: Reduced interdental space in upper lateral incisor region
In the case of virgin adjacent teeth consider orthodontics, a resin-bonded fixed partial denture, or bone augmentation for subsequent implant placement.
Evaluate residual bone height with sufficient bucco-lingual width above the mental foramen and the lower alveolar nerve prior to implant treatment. A majority of posterior mandibular cases require cross-sectional images. Always secure an apical safety distance between the site preparation and nerve structures.
Missing upper bicuspids or molars generally imply downward expansion of the maxillary sinus, which in turn may interfere with conventional implant treatment. The altered anatomy may call for various treatment options such as augmentation procedures or conventional tooth-supported prosthetics.
Beware of apically converging roots of adjacent teeth, which may intervene with implant placement in terms of accidental contact with the periodontal ligament or root cementum. Occasionally the blood vessel entering the apex of a converging root may be cut off during site preparation, resulting in pulp necrosis.
To assess the properly the available bone volume when a single tooth is missing, after the conventional intra-oral radiograph has been examined, cross-sectional imaging may be needed especially in the vicinity of anatomical landmarks such as nerves and vessels.”
