-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Anterior and posterior location considerations
Key points
- In cases of limited bone volume in the single-tooth site consider using narrow platform implants, bone augmentation, orthodontic space closure or tooth-supported prosthetics.
- Evaluate lip line, soft tissue level and presence/absence of papillae in the esthetic zone.
- Observe relevant nerve and vessel structures and other anatomic landmarks during surgery.
General considerations
Missing single teeth imply a variety of bone sites for implant placement. Incisor regions are frequently impeded by inadequate mesio-distal and/or bucco-lingual bone dimensions, whereas second bicuspid/molar regions are generally affected by inadequate vertical bone dimensions.
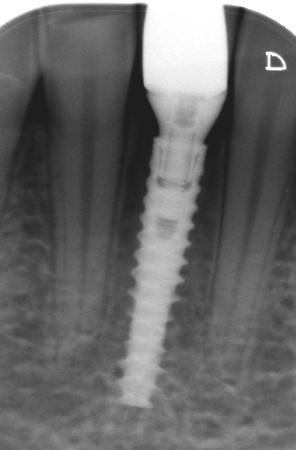
Preoperative evaluation must include radiographs and, based on individual decision making, cross-sectional imaging (CBCT, CT) should be considered.
Anterior region maxilla
Replacing a missing central incisor with an implant may be jeopardized or even impossible due to a short distance between the lateral incisor and the maxillary suture or between the lateral incisor and the nasopalatine foramen.
The lateral incisor region presents regularly with diminished mesio-distal and bucco-lingual bone dimensions.
The buccal bone tissue contour may be compromised in terms of concavities, depending on cause for and timing of a missing upper incisor or canine. The lip line position will have a high impact on the esthetic appearance.
An avulsed repositioned injured tooth will frequently develop root resorption and ankylosis, resulting in infra-position. In this case, implant treatment will in general then require bone and soft tissue augmentation.

Anterior region mandible
Replacing a missing central/lateral incisor with an implant is often not possible due to insufficient mesio-distal and bucco-lingual bone dimensions.
Implant treatment in in such jaw bone could seriously jeopardize the bone support of adjacent teeth.
An extra narrow diameter implant may save the situation (Fig 4), whereas alternative treatments involve orthodontic space closure or resin-bonded fixed partial dentures.
Posterior regions maxilla and mandible
Loss of a bicuspid or a molar in the maxilla often results in expansion of the sinus cavity, which regularly interferes with implant placement.
Cross-sectional images will reveal if the available bucco-lingual bone dimension underneath the sinus is sufficient for an implant (Fig 5). In case of insufficient bone volume, such images will also reproduce the sinus anatomy, which in turn may be helpful when performing bone augmentation.

Apical parts of second bicuspid and molar sites in the mandible approach the mental foramen and the lower alveolar nerve, respectively.
Cross-sectional imaging is strongly recommended to verify available bone height above nerve structures and any presence of a submandibular gland fossa.
Make sure to have at least 1 mm of bone between the osteotomy and the mental foramen/lower alveolar nerve.
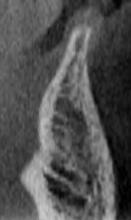
An anterior loop of the lower alveolar nerve in relation to the mental foramen may occasionally be present (Fig 6). Accidental contact with the loop during site preparation may result in permanent nerve damage.

Both maxilla and mandible tend to show less dense bone texture posteriorly, thus often requiring an adapted drill protocol (under-preparation of the osteotomy).
A missing upper/lower molar should preferably be replaced by a wide platform implant (Ø ≥5mm).