-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
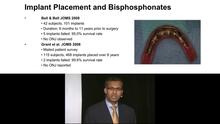
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
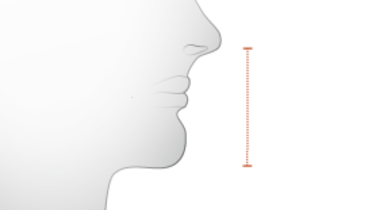
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Alveolar atrophy and insufficiency
Key points
- Alveolar ridge reduction/resorption is influenced by local, systemic and genetic factors
- Frequent use of 2-D imaging to evaluate residual edentulous bone reveals better height than width assessment
- Implant-supported prostheses, unlike complete dentures, appear to retard the ongoing bone resorption
Alveolar ridge resorption / reduction
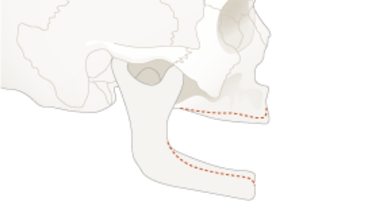
Teeth extractions are followed by a reduction of the bucco-lingual as well as the vertical dimension of the residual alveolar ridge. The ensuing resorption is progressive and even the basal jaw may become involved. In the lower jaw, the mandibular nerve can become located on top of the crest, causing pain to denture wearers.
Reduction of alveolar ridge height is far more frequently encountered in edentulous mandibles than in edentulous maxillae. Longevity of denture wearing, gender and a diminished Body Mass Index are associated with increased ridge resorption, while age does not appear to be relevant. Osteoporosis has not yet been shown to significantly influence alveolar ridge resorption, while recent research from specialized centers suggests that identified genetic factors can determine such bony changes.
Inserting endosseous implants to retain/support a dental prosthesis retards further jaw bone resorption. When alveolar ridge resorption is advanced, clinical and specific imaging examinations will inform the doctor which remaining jaw bone areas are still available for the optimal placement of short/narrow endosseous implants. This scrupulous evaluation can lead to avoidance of invasive bone augmentation procedures.
Alveolar insufficiency
Patients with ectodermal dysplasia and anodontia, or patients with a cleft palate syndrome can have an alveolar insufficiency. The absence of teeth prevents the development of proper jaw bone dimensions and the associated available bone volume often does not allow placement of endosseous implants without prior bone augmentation procedures. Part of the diagnosis is to determine the skeletal age and growth to determine the timing of implant placement.
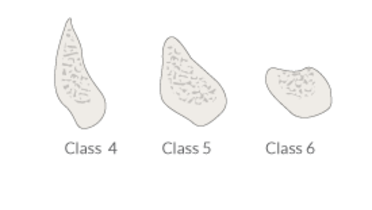
Alveolar insufficiency may also refer to the bone quality. The maxillary tuberosity for example, consists mainly of marrow spaces and adipose tissue and female patients demonstrate in general a lower amount of mineralized bone trabeculae. Distal mandibular sites may also reveal extremely poor bone mineralization. Spiral CT scans permit bone density quantification in Hounsfield Units, although bone density measurements on CBCT images are less reliable.