-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
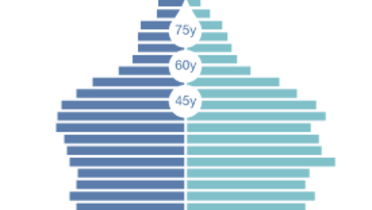
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
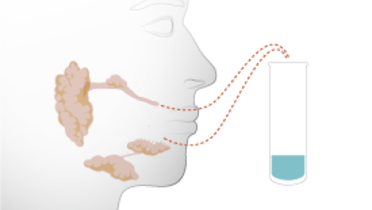
Salivary output
Key points
- Physiological salivary output is 0.75 to 1.5 liters per day
- Distinguish salivary output at rest and when stimulated. Salivary output testing is easy to accomplish
- Xerostomia interferes with wearing of mucosally-borne prostheses like complete dentures
Saliva as a multi-functional solution
Physiological salivary output is 0.75 to 1.5 liters per day, with most originating from the submandibular glands. Saliva is a lubricant and has a complex set of protective and healing functions for the oral cavity. It adheres instantly to mucosa as a transparent pellicle consisting of low-molecular weight mucins and proteins with antimicrobial properties and cystatins that regulate inflammatory conditions and histatins that are potent antifungals. Saliva also contains lactoferrin that inhibits microbial growth, and epidermal growth factor that favors tissue healing and amylase to aid in digestion. Clearly, saliva is a multi-functional solution.
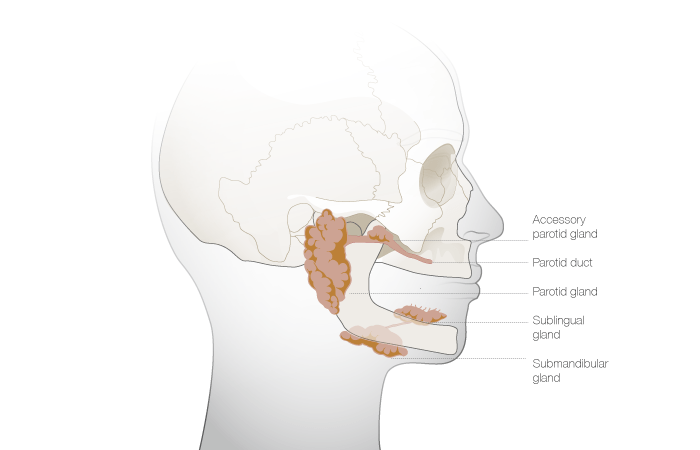
Hyposalivation
Hyposalivation refers to the condition of reduced salivary output and is more often seen in the elderly because it is a side effect of many medications. Hyposalivation is also observed in patients suffering from Sjogren's syndrome. Xerostomia refers to the patient's perception of reduced salivary output and resulting perceptible debilitations such as a feeling of dry mouth. A reduction of salivary output by 50% is suggested to be a typical threshold at which patients perceive xerostomia. Decreased salivary flow predisposes to superinfections and impairs oral functions like chewing and speaking, and by extension, decreases quality of life. In patients who wear complete dentures and are affected by xerostomia, an implant-based rehabilitation may be of benefit to stabilize a prosthesis.
Salivary output testing
Measuring salivary output is relatively easy. The drooling test reveals the total salivary ouptut ( 0.1 – 0.5 ml/min at rest). More simple tests exist such as measuring the weight loss of a standard hard sugar candy, held passively for 3 minutes between tongue and palate, or chewing a dry gauze for 2 minutes and calculating weight gain. Pathological output at rest is considered to be < 0.1 ml/min; while during stimulation, < 0.5 ml/min is considered pathological. In these situations, the clinician should check for Sjögren disease, medications linked to xerostomia like antidepressants, diuretics, antihistamines and antihypertensives. In addition, a history of radiotherapy to the salivary glands can significantly reduce salivary flow.
Saliva substitute options
The use of saliva substitutes is enjoyed by some, but not all, patients and medications, such as pilocarpine, or drinking green tea are recommended to stimulate salivary flow.