-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
General patient history
Key points
- Review general health status of patient, medication and previous surgeries/treatments
- Evaluate potential interferences with planned or likely treatment
- In case of doubt seek general medical / internist’s advise
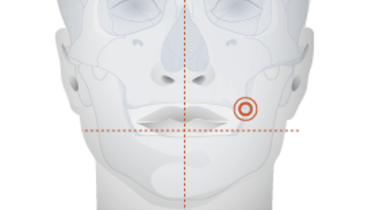
Initial assessment - Patient interview
It is helpful if a clinician is situated so that his/her eyes are at the level of the patient's eyes. For example, if the patient is seated, the clinician should also be seated. It is beneficial if the interview between clinician and patient does not occur in a dental chair as this will not facilitate confidence. In this way, key aspects of the patient's personality, expectations, and medical conditions are more likely to be shared. It is vital that the patient's chief complaint be identified to be later matched with his treatment expectations. All patient interview procedures should ensure patient privacy.
General health assessment
A general health assessment should review the following biological systems:
- Cardio-vascular
- Blood
- Neural
- Gastro-intestinal
- Urogenital
- Metabolic diseases
- Previous surgeries and hospital visits
- Allergies, skin (especially allergies to substances found in dental (restoration) materials)
- Infections, specific infections (Hepatitis, HIV)
- Head and neck conditions including angiomata, nasal or sinus surgery and laryngeal or oro-pharyngeal complaints
In addition, one should inquire about a history of travel to tropical countries (latency of certain diseases). It may be necessary to procure medical reports if available. In case of doubt consider referring patient to the house doctor or internist for further evaluation or recommendations.
Also, consider inquiring/assessing about use of nicotine, alcohol, drugs (Refer also to chapter ‘risk assessment’).
Medication
Reviewing the medications that the patient is currently taking, or has taken in the past, may identify risks to surgical and prosthetic treatment. Furthermore, a patient may not always know the conditions for which they are being treated and their medication list may signal additional conditions of concern to be investigated by the clinician. For example, elderly patients consider medication a routine and might forget to mention them, if asked in a generic way. In case of doubt ask patients if they take any medication for the bone, for the heart and so on.