-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Radiotherapy
Key points
- Implant-based treatment in radiated bone is possible and often the preferred way to provide a functional restoration
- Doses above 55 Gy (Gray) interfere critically with osseointegration
- Adequate antibiotic therapy and eventually hyperbaric oxygen may prevent osteoradionecrosis
- Due to functional limitations, oral hygiene home care and need for checking cancer recurrences, consider removable prostheses/obturators
Radiotherapy
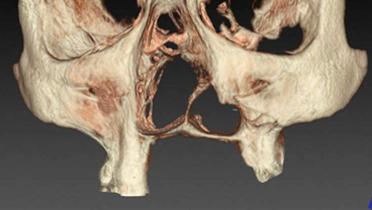
Rehabilitation of patients with oral cancers is usually done in a combined way with surgical, chemo- and radio-therapy. Radiotherapy predisposes to fibrotization, ischemia and xerostomia. The latter side-effect renders mucosally supported dentures even more difficult to wear.
Implant-based restoration options
There is clinical evidence that implants can successfully be inserted in radiation-treated bone. Meta-analysis revealed a failure rate of <5 % in the mandible. Long-term implant survival rates seem however to be reduced, and may influence treatment expectations, in the context of the estimate survival time for a patient.
It has been suggested that implant surgery be postponed for 9-12 months after radiation therapy but data to support this are scarce. Therefore, in order to offer the patient earlier rehabilitation, the length of postponement may be shortened if clinical circumstances which indicate that bone healing potential is sufficient.
Clinicians should consider a two-stage surgical protocol to avoid implant site infection and to promote undisturbed osseointegration. In addition, osseointegration in radiated bone is considerably slower. Hyperbaric oxygen therapy may be useful. In all surgical scenarios, antibiotic protection to prevent infected osteoradionecrosis is critical.
Patients should be informed about therapy staging. In case of osteo-myo-cutaneous transplant reconstructions of the mandible, consider implant insertion after healing period of the transplant (usually 3 months). Reopening surgery is recommended after another 3 months and may need to be combined with a vestibuloplasty to model the soft tissue of the transplant.
Due to the functional limitations of the radiated patient, rehabilitation may not achieve the same overall functional level as in a healthy patient. Patients should be informed of the likely compromise during the treatment planning phase in order to set reasonable treatment outcome expectations.