-
0
Patient Assessment
- 0.1 Patient Demand
- 0.2 Anatomical location
-
0.3
Patient History
- 2.1 General patient history
- 2.2 Local history
-
0.4
Risk Assessment
- 3.1 Risk Assessment Overview
- 3.2 Age
- 3.3 Patient Compliance
- 3.4 Smoking
- 3.5 Drug Abuse
- 3.6 Recreational Drug and Alcohol Abuse
- 3.7 Condition of Natural Teeth
- 3.8 Parafunctions
- 3.9 Diabetes
- 3.10 Anticoagulants
- 3.11 Osteoporosis
- 3.12 Bisphosphonates
- 3.13 MRONJ
- 3.14 Steroids
- 3.15 Radiotherapy
- 3.16 Risk factors
-
1
Diagnostics
-
2
Treatment Options
-
2.1
Treatment planning
- 0.1 Non-implant based treatment options
- 0.2 Treatment planning conventional, model based, non-guided, semi-guided
- 0.3 Digital treatment planning
- 0.4 NobelClinician and digital workflow
- 0.5 Implant position considerations overview
- 0.6 Soft tissue condition and morphology
- 0.7 Site development, soft tissue management
- 0.8 Hard tissue and bone quality
- 0.9 Site development, hard tissue management
- 0.10 Time to function
- 0.11 Submerged vs non-submerged
- 0.12 Healed or fresh extraction socket
- 0.13 Screw-retained vs. cement-retained
- 0.14 Angulated Screw Channel system (ASC)
- 2.2 Treatment options esthetic zone
- 2.3 Treatment options posterior zone
- 2.4 Comprehensive treatment concepts
-
2.1
Treatment planning
-
3
Treatment Procedures
-
3.1
Treatment procedures general considerations
- 0.1 Anesthesia
- 0.2 peri-operative care
- 0.3 Flap- or flapless
- 0.4 Non-guided protocol
- 0.5 Semi-guided protocol
- 0.6 Guided protocol overview
- 0.7 Guided protocol NobelGuide
- 0.8 Parallel implant placement considerations
- 0.9 Tapered implant placement considerations
- 0.10 3D implant position
- 0.11 Implant insertion torque
- 0.12 Intra-operative complications
- 0.13 Impression procedures, digital impressions, intraoral scanning
- 3.2 Treatment procedures esthetic zone surgical
- 3.3 Treatment procedures esthetic zone prosthetic
- 3.4 Treatment procedures posterior zone surgical
- 3.5 Treatment procedures posterior zone prosthetic
-
3.1
Treatment procedures general considerations
-
4
Aftercare
Soft tissue condition
Key points
- Gingival biotypes may relate to soft tissue recessions and crestal bone loss.
- Evidence supporting the need for keratinized mucosa to maintain health around implants is limited, albeit its absence is associated with more plaque accumulation, mucosal recession, and attachment loss.
Gingiva
The gingiva is tightly connected to the underlying periosteum. It is globally keratinized and has a stippled surface. Its color varies from pink to brown or even black, depending on race and/or melanin deposits. It can be distinguished from alveolar mucosa, which is not keratinized, shiny and red, with a visible vascular supply.
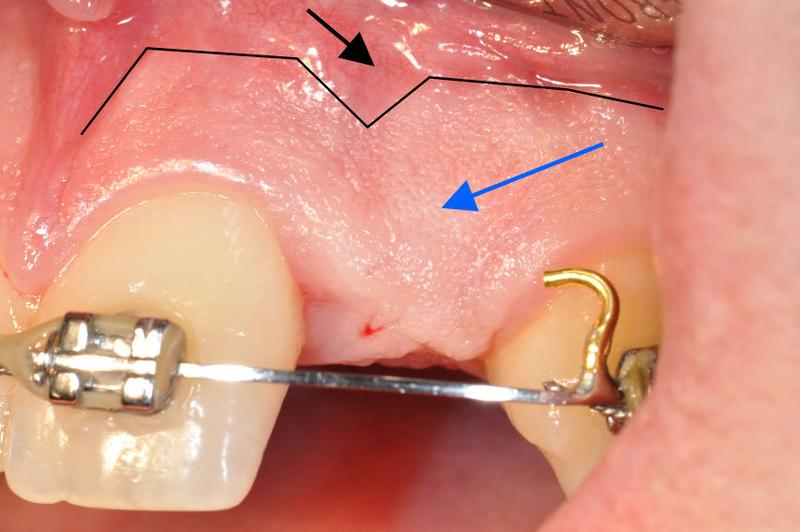
Figure 1: Gingiva – pink colored keratinized with a stippled surface (blue arrow). Muco-gingival junction (black line). Alveolar mucosa – non-keratinized, shiny red appearance (black arrow)
Gingival width and biotype
In both jaws the gingival width is labially narrower in canine/first premolar areas.
Gingival width can be determined by eye inspection or by moving the alveolar mucosa towards the gingiva by applying shear forces with a finger or a periodontal probe put horizontally flat on the mucosa. A ripple is thus created, indicating the muco-gingival junction.
A thin gingival biotype, < 1.5 mm of gingivial thickness, seems more prone to crestal bone loss around implants, but the co-variable "thin labial plate" plays a role. Determining gingival thickness can be done by probing perpendicularly to the gingival surface.
Figures 2 & 3: Labially thin gingival biotype in canine (thin white arrow) and bicuspid regions (black arrows). Labial fold (thick white arrow). Figure 4: Canine presented with the thick biotype (blue arrows)
Lingually the gingival width increases in the dorsal direction in the mandible while the maxilla is entirely covered by keratinized tissue. Many call the keratinized tissue in the absence of teeth masticatory mucosa instead of gingiva. One should not confuse the gingival width with the vestibular depth also called labial fold.
Figures 5 & 6: Palatal maxillary keratinized tissue punched out to improve adaptation towards the implant/abutment.
Clinical evidence on the need for keratinized tissues around implants to maintain tissue health and stability is limited. Gingival widths of ≤ 2 mm are regularly associated with higher plaque and bleeding scores, so a lack of keratinized mucosa seems related to inproper oral hygiene. Most studies report no effect on probing depths. It is important to recognize that the notion that keratinized tissue should be present or created around natural teeth has long been abandoned.










