-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
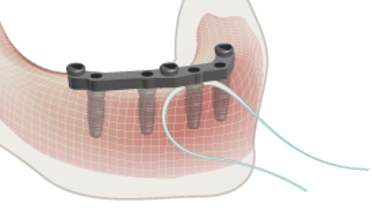
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Overarching considerations
Key points
- Complete edentulism can be a handicap, comparable to other amputations
- Treatment planning should not be imposed, but modulated according to patient wishes, expectations and affordability
- Success depends on many factors. Patients’ adaptability and perception play a key role
How to reach a proper quality of life?
The primary goal is a proper oral function. This implies not only chewing but also speaking, smiling.
Patients’ adaptability varies enormously. Some are satisfied with removable dentures, others object to the esthetics of prostheses, even when invisible to the outer world, since hided by their lips.
The doctor will not impose his viewpoints, but try to meet the patient’s expectations, considering general and local pathologies, age, professional/social background, self-esteem, and financial implications.
The more the proposed treatment comes close to the patient demand, the more the patient is informed about the treatment steps and long-term perspective, the greater the chances for a successful outcome.
Time should be invested into listening to the patient, offering understandable explanations and time for reflection before proceeding any further. Images, such as computer-generated treatment planning, are useful adjuncts. Revealing, the possibly, limited results, eventual complications or even failures, will enhance trust.
How to follow up a treatment?
From day one, the patient should understand that treatment does not end with surgery or the delivery of a prosthetic device. Aftercare meetings are integral part of a treatment.
Coaching the early adaptation to the new situation, will speed up satisfaction. For chewing, one should draw the attention of patients to the new tactile sensation offered by implants.
If speech is a problem, a few months of adaptation or logopedic treatment must be considered. For esthetics, the patient should always evaluate the result in a functional mode: while speaking, smiling … not with lip retracted.
Long-term maintenance care will reinforce factors which contribute to the patient well-being and avoid a downhill trend, when problems occur and additional treatment may be necessary.