-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
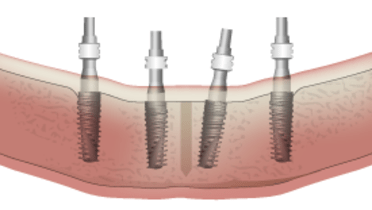
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
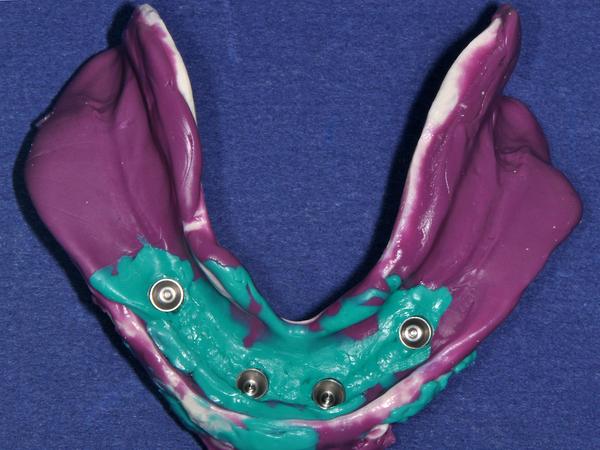
Splinted vs unsplinted impression copings
Key points
- The use of either splinted or unsplinted copings is a matter of personal preference
- In general, although in vitro studies indicate more accurate casts are obtained with splinted impression copings, the increased accuracy does not appear to have clinical significance
- Some clinicians splint impression copings so they can use the connected copings as a verification jig
Splint material selection and accuracy considerations
In vitro research studies have compared splinted versus unsplinted impression techniques and have, in general, shown that the splinted impression technique yields more accurate master casts when compared to a reference model on which the impressions were made. A variety of techniques for splinting have also been evaluated ranging from use of autopolymerizing resin, impression plaster and metal splinting with the overall finding that all three techniques can improve the accuracy of the resulting master cast. However, if autopolymerizing resin is used, its polymerization shrinkage should be minimized by sectioning and reapplication of resin to ensure that the last polymerization involves the smallest volume possible.
Clinical outcomes and clinician preference
Clearly, the most important question is whether clinical outcomes are improved and there is no compelling evidence to date that impressions made using the unsplinted technique lead to a compromised prosthesis and poorer long-term clinical outcomes. Hence, the decision to splint or not splint impression copings is ultimately one of personal preference of the clinician since additional materials and extra chair time are required when the splinted technique is utilized. Also, some clinicians use the splinted copings as a verification jig which may be of sufficient clinical advantage to use this technique along with the improved master cast accuracy obtained. A brief outline of the clinical technique and pertinent considerations are presented below.
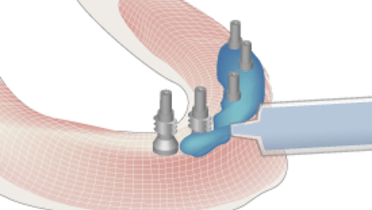
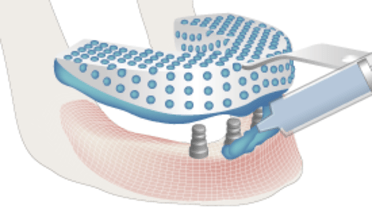
When open tray impression copings are used, the clinician has a choice between splinting or keeping the open tray impression copings unsplinted. The primary purpose of splinting by some clinicians is to gain additional stability of the connected copings in the impression when the abutment analogs are attached.