-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Muco-gingival junction
Key points
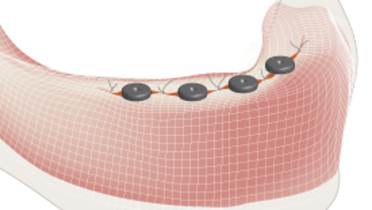
- Determining the width of keratinized tissue is an important consideration when planning possible implant locations
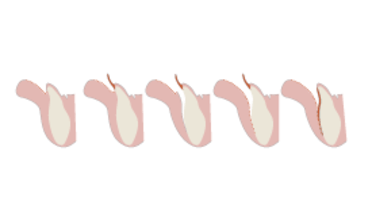
- Gingival biotypes may relate to soft tissue recessions and crestal bone loss
Gingiva
The gingiva is tightly connected to the underlying periosteum. It is globally keratinized and has a stippled surface. Its color varies from pink to brown or even black, depending on race and/or melanin deposits. It can be distinguished from alveolar mucosa, which is not keratinized, shiny and red, with a visible vascular supply.
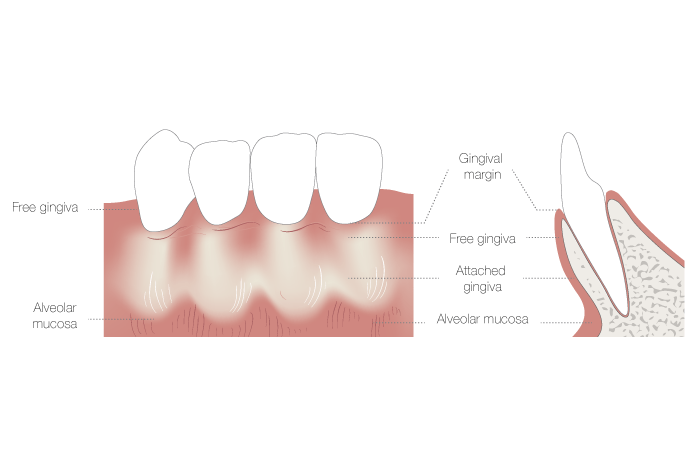
Gingival width and biotype
The gingival width reduces along with the degree of jaw bone resorption in case of edentulism.
In both jaws the gingival width is labially narrower in canine/first premolar areas. Lingually it increases in the dorsal direction in the mandible while the maxilla is entirely covered by keratinized tissue. Many call the keratinized tissue in the absence of teeth masticatory mucosa instead of gingiva. One should not confuse the gingival width with the vestibular depth also called labial fold.
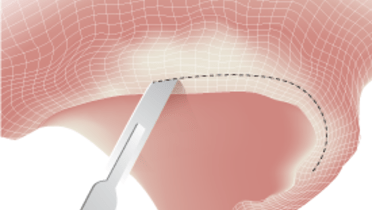
Gingival width can be determined by eye inspection or by moving the alveolar mucosa towards the gingiva by applying shear forces with a finger or a periodontal probe put horizontally flat on the mucosa. A ripple is thus created, indicating the muco-gingival junction.
A thin gingival biotype, < 1.5 mm of gingivial thickness, seems more prone to crestal bone loss around implants, but the co-variable "thin labial plate" plays a role. Determining gingival thickness can be done by probing perpendicularly to the gingival surface, by radiographs or an ultrasonic device, although the latter is not easily found commercially.
Clinical evidence on the need for keratinized tissues around implants to maintain tissue health and stability is limited. Gingival widths of ≤ 2 mm are regularly associated with higher plaque and bleeding scores, so a lack of keratinised mucosa seems related to inproper oral hygiene. Most studies report no effect on probing depths. It is important to recognize that the notion that keratinized tissue should be present or created around natural teeth has long been abandoned.