-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Comprehensive treatment concepts, Zygomatic implants
Key points
- Zygomatic implants have been an evidence-based surgical and prosthetic solution for nearly two decades (using the two-stage approach)
- Since 2007 zygomatic implants have been proven to work in the immediate function protocol
- In severely resorbed clinical situations, zygomatic implants are the only option to rehabilitate the patient immediately
- Zygomatic implants are a proven alternative to bone grafting
- Careful attention to treatment planning will facilitate a more straight-forward prosthetic reconstruction
Bone volume deficiencies - augmentation or zygomatic implants options
Conventional dentures are a common treatment option, but, when bone is missing, they may not meet functional, psychological and social needs of the individual. Classical surgical approaches include different bone augmentation techniques (sinus lift, onlay grafts and LeFort I osteotomy with interpositional grafts). Over the past years promising results have been published using biomaterials for bone regeneration. Nevertheless, the need for delayed protocols, the potential for intra- and extraoral complications and the patient compliance needed, influence the acceptance rate for these techniques, especially when a previous therapy has failed.
When bone volume deficiencies are present, zygomatic implants should be considered as an alternative to conventional bone grafting. High longterm success rates using the classical 2-stage protocol and immediate loading have been published. Furthermore, the extrasinus approach has been published.
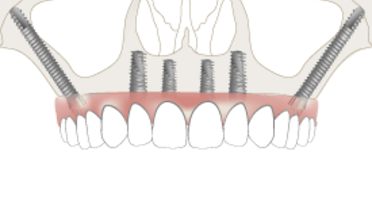
For the totally atrophied maxilla, the concept has been expanded to anchoring 2 additional implants in each zygomatic bone: by means of 4 well-distributed zygomatic implants a fixed bridge is immediately loaded (Quad zygoma approach).
Indications and contra-indications for zygomatic implants
Indications include:
- totally atrophied maxilla Cawood V/VI (Quad zygoma approach)
- totally edentulous maxilla, when the posterior alveolar crest has resorbed to such an extent that additional implants would require support of onlay/inlay grafts (two regular and two zygomatic implants recommended)
Zygomatic implants are especially recommended in:
- end of the line treatment after failed implant treatment or failed graft/maxillectomy cases
- when immediate function is the treatment priority
Contraindications include:
- acute sinus infection
- maxillary/zygoma pathology
- underlying uncontrolled/malignant systemic disease
Diagnostic considerations
In order to correctly treatment plan for zygoma implants, the clinician must carefully examine the patient. Consider 3 clinical key aspects:
- type of defect
- smile line and its impact on the transition zone
- analysis of the skeletal relationship between the jaws
Prosthetic rehabilitation
When it comes to prosthetic rehabilitation, there are not many differences between fixed prostheses on regular implants and a fixed rehabilitation using zygomatic anchorage because the emergence of the implants in both cases is crestal. A fixed prosthesis splints all the implants avoiding relative motion of the zygoma implants. Originally, a 2-stage approach was used. Today it is recommended to use a cross-arch stabilisation prosthesis to immediately load the implants.
Depending on the patient’s wish and maintenance capabilities the following restorations are recommended:
- fixed: NobelProcera Implant Bridge on implant or abutment level as 1st choice
- fixed-removable: NobelProcera Implant Bar Overdenture
Treatment examples using zygomatic implants
1 Rehabilitation of the severly resorbed maxilla with four zygomatic implants
This patient presented with a totally resorbed maxilla and has never received implant-supported treatment before. Four zygomatic implants have been placed in the upper jaw and the existing removable dentures have been converted into fixed implant-supported prostheses for both the upper and lower jaws.










What can I do about my gums receding around the abutments?
I had the zygomatic surgery a year and a half ago.
I had the zygomatic surgery a year and a half ago.