-
0
Patient Assessment
- 0.1 Patient demand
- 0.2 Overarching considerations
- 0.3 Local history
- 0.4 Anatomical location
- 0.5 General patient history
-
0.6
Risk assessment & special high risk categories
- 5.1 Risk assessment & special high risk categories
- 5.2 age
- 5.3 Compliance
- 5.4 Smoking
- 5.5 Drug abuse
- 5.6 Recreational drugs and alcohol abuse
- 5.7 Parafunctions
- 5.8 Diabetes
- 5.9 Osteoporosis
- 5.10 Coagulation disorders and anticoagulant therapy
- 5.11 Steroids
- 5.12 Bisphosphonates
- 5.13 BRONJ / ARONJ
- 5.14 Radiotherapy
- 5.15 Risk factors
-
1
Diagnostics
-
1.1
Clinical Assessment
- 0.1 Lip line
- 0.2 Mouth opening
- 0.3 Vertical dimension
- 0.4 Maxillo-mandibular relationship
- 0.5 TMD
- 0.6 Existing prosthesis
- 0.7 Muco-gingival junction
- 0.8 Hyposalivation and Xerostomia
- 1.2 Clinical findings
-
1.3
Clinical diagnostic assessments
- 2.1 Microbiology
- 2.2 Salivary output
-
1.4
Diagnostic imaging
- 3.1 Imaging overview
- 3.2 Intraoral radiographs
- 3.3 Panoramic
- 3.4 CBCT
- 3.5 CT
- 1.5 Diagnostic prosthodontic guides
-
1.1
Clinical Assessment
-
2
Treatment Options
- 2.1 Mucosally-supported
-
2.2
Implant-retained/supported, general
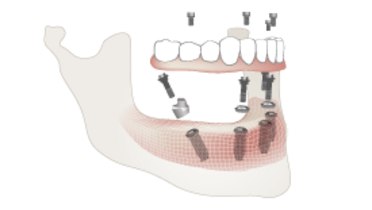
- 1.1 Prosthodontic options overview
- 1.2 Number of implants maxilla and mandible
- 1.3 Time to function
- 1.4 Submerged or non-submerged
- 1.5 Soft tissue management
- 1.6 Hard tissue management, mandible
- 1.7 Hard tissue management, maxilla
- 1.8 Need for grafting
- 1.9 Healed vs fresh extraction socket
- 1.10 Digital treatment planning protocols
- 2.3 Implant prosthetics - removable
-
2.4
Implant prosthetics - fixed
- 2.5 Comprehensive treatment concepts
-
3
Treatment Procedures
-
3.1
Surgical
-
3.2
Removable prosthetics
-
3.3
Fixed prosthetics
-
3.1
Surgical
- 4 Aftercare
Veneering with Ceramic
Key points
- With minimal bone resorption, a ceramo-metal restoration is the preferred choice to accommodate interarch space limitations
- Ceramic veneering provides optimal esthetics and wear resistance and facilitates hygiene
- To minimize chipping risks, adequate anatomical design of the framework allowing appropriate porcelain thickness is important
General considerations and material selection
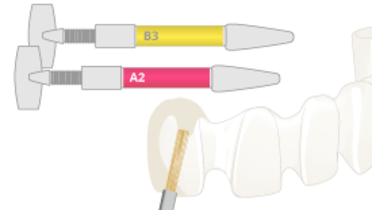
Frameworks can be made from titanium, zirconia, precious alloys and Co-Cr base alloys and can be cement-retained or screw-retained. With minimal bone resorption, a ceramo-metal restoration is preferable to accommodate interarch space limitations. CAD/CAM milling of the frameworks is nowadays considered state-of-the-art. The framework is veneered with veneering materials to complete esthetics and shape of the definitive restoration. There are various ceramic veneering material options available, mainly based on glass or feldspathic ceramics, with a broad selection of tooth shades and gingival colors for optimal esthetics. Veneering with ceramics provides highly esthetic restorations, guarantees smooth surfaces with low plaque accumulation, good oral hygiene and patient comfort. Veneering ceramics can be veneered onto the framework by manual layering or pressing techniques.
Guidelines
For stability of the veneering ceramics and ideal support by the framework, the framework design and shape should mimic the design of the final restoration to allow for an even thickness of the ceramic veneering layer. To provide sufficient esthetic veneering options, the component selection and anatomical framework design should allow for a 1.2 - 1.5 mm veneering thickness. Highly polished/glazed surfaces are crucial, especially for surfaces facing the mucosa.
In case of a screw-retained restoration, the access to the screw channel will go through the framework structure and the veneering layer. Depending on location and design of the screw access opening, after seating the restoration it might be beneficial to close the opening to avoid food impaction and damage. This is typically closed with a light-curing composite material. To facilitate removal of the composite and to protect the screw when accessing the channel with a rotating instrument for maintenance of the restoration, the composite is placed over a soft layer of for example teflontape, guttapercha or a cotton pellet.
Potential complication aspects
The bonding mechanism between zirconia and the veneering ceramic is not yet well-known and the framework-veneering ceramic interface is among the weakest aspects of these restorations, so chipping can occur and is a potential and most typical complication. Adequate design of the anatomically designed framework with appropriate porcelain thickness is important. Several techniques have been developed to address potential chipping of the porcelain layer, such as the 'overpressing technique', which improves the homogeneity and density of the layering materials. It can be considered to not veneer the oclusal surface and leave it in zirconia. In case of chipping, the easy retrievability of the screw-retained restoration is a major advantage.
After intra-oral adjustments with a rotating instrument it is crucial to polish the ceramic surface for patient comfort and to reduce the risk of cracks induced by the irregularities of the cut ceramic surface. After such adjustments it is even recommended to glaze the ceramic restoration surface again in the laboratory.
After extended periods of intraoral use (months), due to conversion effects of the veneering ceramic in the intraoral environment, there is only limited technical potential to successfully change and refire the ceramic. Therefore after placement of the restoration any required adaptations should be identified and executed as soon as possible.