-
0
Introduction and Importance of Peri-implant Soft Tissue
00:00 - 03:27
-
1
Role of Peri-implant Mucosa in Implant Protection
03:28 - 06:24
-
2
Innovations in Implant Surfaces and Components
06:25 - 13:55
-
3
Importance of Mucosa Quality and Quantity
13:56 - 19:38
-
4
Monitoring and Manipulating Peri-implant Mucosa
19:39 - 23:00
- 5 Community questions
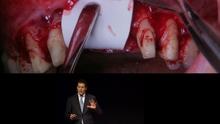
Achieving Predictable Long Success through Peri-implant Soft Tissue Management: When, Why, How. Part 1
Video highlights
- Critical Role of Peri-implant Soft Tissue
- Sealing Function of the Mucosa
- Innovative Implant Surfaces for Muco-integration
- Why Mucosal Thickness Matters
- Digital Tools & Techniques for Tissue Shaping
Dr. Tabanella begins his presentation with a compelling introduction to the often-underappreciated realm of peri-implant soft tissue management. From the outset, he underscores its essential role in the overall success and longevity of dental implants. Rather than viewing soft tissue as a secondary factor, he positions it as a biological barrier and a critical determinant of both functional and aesthetic outcomes.
He explains that unlike natural gingiva, the peri-implant mucosa lacks certain structural elements, making it more vulnerable to bacterial invasion. As such, the design and preservation of a healthy soft tissue collar around implants is not merely beneficial—it is imperative. Dr. Tabanella describes how even small compromises in this collar can result in long-term biological complications, emphasizing the need for "soft tissue boosting" strategies before and after implant placement.
Moving deeper into the biological nuances, he outlines the distinct anatomy of peri-implant mucosa, highlighting differences in collagen fiber orientation, vascular supply, and epithelial attachment compared to natural teeth. These differences, he notes, directly influence how the tissue behaves in response to mechanical stress, plaque, and surgical manipulation.
The presentation then pivots to focus on the protective function of the peri-implant mucosa. Dr. Tabanella methodically explains how this soft tissue acts as a seal to prevent bacterial contamination from penetrating the underlying bone and implant surface. He emphasizes that once this seal is broken—whether due to poor surgical technique, prosthetic misfit, or inflammation—the implant becomes vulnerable to mucositis and potentially irreversible peri-implantitis.
He shares clinical cases and statistical data to show the consequences of a compromised mucosal barrier, revealing how quickly inflammation can escalate if early warning signs are ignored. Maintaining this seal is not a passive task, he asserts, but requires continuous assessment and thoughtful intervention at every stage of the treatment plan.
As the lecture progresses, Dr. Tabanella introduces cutting-edge developments in implant surface technology that are aimed at optimizing soft tissue integration. He details innovations such as the TiUltra surface, which offers improved interaction with peri-implant tissues. He also discusses sealed surface technology, which facilitates keratinocyte migration and encourages the formation of a more stable soft tissue interface.
These innovations reflect a shift in implantology—from focusing solely on osseointegration to also emphasizing muco-integration, a term he uses to describe the intentional integration of soft tissue with implant components. He explains how anodized surfaces, in particular, have shown promise in enhancing the biological seal and reducing microbial colonization at the abutment level.
The focus then transitions to the quality and quantity of the peri-implant mucosa. Dr. Tabanella explains that a thicker mucosal biotype not only contributes to better aesthetics but also helps in preventing bone loss. He illustrates the correlation between mucosal thickness and bone resorption, showing that implants surrounded by thin or insufficient soft tissue are far more prone to long-term failure.
He stresses the value of keratinized mucosa in controlling plaque accumulation and reducing the risk of inflammation. Citing clinical research and his own experience, he makes a strong case for augmenting soft tissue in cases where keratinized tissue is lacking, particularly in the anterior zone where esthetic demands are high.
As he nears the conclusion of the talk, Dr. Tabanella explores modern techniques for monitoring and manipulating peri-implant soft tissue. He introduces digital soft tissue scanning, which allows for non-invasive monitoring of tissue contours over time. This technology, he says, is revolutionizing how clinicians track subtle changes in peri-implant health.
Equally important are the techniques used to manipulate and shape the soft tissue during and after implant placement. He elaborates on the role of provisional restorations as tools not just for function and aesthetics, but for actively guiding the maturation and architecture of the soft tissue. In his view, every stage of implant therapy—surgical, prosthetic, and maintenance—must prioritize the preservation and enhancement of the peri-implant mucosa.
In wrapping up, Dr. Tabanella reiterates that successful implant outcomes are not solely about osseointegration or prosthetic craftsmanship. Instead, they depend on the ongoing health and stability of the surrounding soft tissue. He calls on clinicians to adopt a more biologically driven approach, integrating new technologies and refined techniques to support the dynamic and protective role of peri-implant mucosa.
Through his detailed and data-supported narrative, Dr. Tabanella presents soft tissue management not as a secondary consideration, but as the foundation of modern implantology. His presentation leaves the audience with a deeper appreciation for the biological complexity of the peri-implant environment and a clear call to elevate the standards of care in this critical area.