-
0
Introduction
00:00 - 00:46
-
1
Defining success in peri-implantitis management
00:47 - 02:39
-
2
Lessons learned in peri-implantitis management
02:40 - 04:18
-
3
Peri-implant defect configuration
04:19 - 05:59
-
4
Step-by-step approach for Class 1 defects
06:00 - 10:48
-
5
Step-by-step approach for Class 2 defects
10:49 - 12:24
-
6
Step-by-step approach for Class 3 defects
12:25 - 14:56
-
7
Conclusion
14:57 - 15:45
- 8 Community questions
New treatment concepts to prevent and manage peri-implant diseases - part 2 surgical therapy
Video highlights
- Evolution of peri-implantitis management
- Peri-implantitis defect configuration
- Detailed treatment approach for each defect category
How is success defined when treating peri-implantitis? This is one of several important questions addressed by Dr. Monje in his lecture on surgical therapy of peri-implantitis. With his lecture, he aims to simplify the complex decision-making process for a sufficient solution for this disorder.
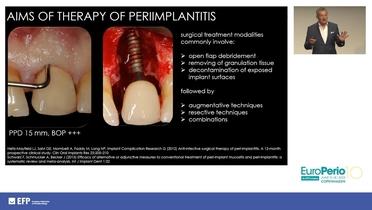
The first step is to define success in peri-implantitis management. Which factors can be qualified and reviewed to determine whether a treatment has been successful? Amongst the success-defining factors are a reduction in probing pocket depth of less than 5mm, no bleeding on probing, and no bone loss. Dr. Monje differentiates peri-implantitis from periodontitis, which presents with a specific development pattern that is very different from that of periodontitis. Gain perspective from his detailed illustration of the various defect configurations that can be exhibited when peri-implantitis is present.
What is the impact of defect type on the rehabilitation potential? And how can it be identified? There are three main defect categories, and each can have up to three subclasses. One commonality shared by most defects is that the buccal wall is affected; this is a crucial point in the prevention of peri-implantitis. Dr. Monje reviews each defect configuration and explains the options to bring this defect to an optimal result. The various treatment methods available to treating clinicians are presented with a solid scientific background.
When planning the treatment for a peri-implantitis case, it is important to keep in mind that the ideal combination of two methods can be leading to a successful outcome and rehabilitation of the affected implant. This includes established, well-proven treatment methods as well as new treatment methods, such as electrolytic cleaning, that present additional options to the treatment process.
View part one of this series here with Dr. France Lambert’s introduction to the topic and Dr. Giacomo Fabbri’s discussion on the prosthetic aspects of prevention of peri-implant disease and return to for.org for more episodes in this series.
References
[1] Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, Mealey BL, Papapanou PN, Sanz M, Tonetti MS. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018 Jun;45 Suppl 20:S1-S8. doi: 10.1111/jcpe.12935. PMID: 29926489.
[2] Charalampakis G, Rabe P, Leonhardt A, Dahlén G. A follow-up study of peri-implantitis cases after treatment. J Clin Periodontol. 2011 Sep;38(9):864-71. doi: 10.1111/j.1600-051X.2011.01759.x. Epub 2011 Jul 19. PMID: 21770994.
[3] Monje A, Schwarz F. Principles of Combined Surgical Therapy for the Management of Peri-Implantitis. Clin Adv Periodontics. 2022 Mar;12(1):57-63. doi: 10.1002/cap.10186. Epub 2021 Nov 12. PMID: 34569711.
[4] Schwarz F, Sahm N, Schwarz K, Becker J. Impact of defect configuration on the clinical outcome following surgical regenerative therapy of peri-implantitis. J Clin Periodontol. 2010 May;37(5):449-55. doi: 10.1111/j.1600-051X.2010.01540.x. Epub 2010 Mar 24. PMID: 20374416.
[5] Aghazadeh A, Persson RG, Renvert S. Impact of bone defect morphology on the outcome of reconstructive treatment of peri-implantitis. Int J Implant Dent. 2020 Jun 17;6(1):33. doi: 10.1186/s40729-020-00219-5. PMID: 32548733; PMCID: PMC7297900.
[6] Monje A, Pons R, Insua A, Nart J, Wang HL, Schwarz F. Morphology and severity of peri-implantitis bone defects. Clin Implant Dent Relat Res. 2019 Aug;21(4):635-643. doi: 10.1111/cid.12791. Epub 2019 May 14. PMID: 31087457.
[7] Monje A, Amerio E, Cha JK, Kotsakis G, Pons R, Renvert S, Sanz-Martin I, Schwarz F, Sculean A, Stavropoulos A, Tarnow D, Wang HL. Strategies for implant surface decontamination in peri-implantitis therapy. Int J Oral Implantol (Berl). 2022 Sep 9;15(3):213-248. PMID: 36082658.
[8] Bosshardt DD, Brodbeck UR, Rathe F, Stumpf T, Imber JC, Weigl P, Schlee M. Evidence of re-osseointegration after electrolytic cleaning and regenerative therapy of peri-implantitis in humans: a case report with four implants. Clin Oral Investig. 2022 Apr;26(4):3735-3746. doi: 10.1007/s00784-021-04345-1. Epub 2022 Mar 4. PMID: 35244779; PMCID: PMC8979896.
[9] Monje A, Blasi G, Nart J, Urban IA, Nevins M, Wang HL. Soft Tissue Conditioning for the Surgical Therapy of Peri-implantitis: A Prospective 12-Month Study. Int J Periodontics Restorative Dent. 2020 Nov/Dec;40(6):899-906. doi: 10.11607/prd.4554. PMID: 33151197.