Live Webinar: Maintenance of dental implants
Video highlights
- Set up of successful maintenance plan
- Detailed information on instruments, devices and procedures
With a live webinar, FOR embarks on a new path in providing access to educational content. In this first webinar, presented by Dr. Miguel de Araújo Nobre and moderated by Dr. Susan Tanner, we learn about an optimal maintenance plan to support the success of an implant rehabilitation.
Dr. Tanner starts the webinar by welcoming all participants and informing them how to address questions during the presentation. She introduces the speaker of the webinar, Dr. Miguel de Araújo Nobre and hands over to him. During this lecture, Dr. Nobre will give us a glimpse of the key points that they consider important to achieve success and to maintain it over the long-term. He explains that his lecture is separated into two phases as is the maintenance, the first phase of maintenance and the second phase of maintenance. And in the third part of this lecture, he will discuss a little bit about the threats to long-term success while we will be able to check some new tools that they have both for risk score in peri-implant pathology and a prognostic model. In 2019, they were able to publish on the success of the All-on-4 concept over 20 years, considering that the All-on-4 is a three arms monster with surgery, prosthodontics, and maintenance, and they don't consider any arm more important than the other. All of them are considering equally important. We may have an excellent set of implants placed, but if our prosthesis doesn't match, then we're going to have trouble. Or even if we have good surgery, good prosthodontics, but then no maintenance, it's just a matter of time until a problem will occur, and the patient will come back complaining. To keep the excellence that we achieve when we place an immediate functional prosthesis, we need to separate maintenance into two phases. First phase is the functional osseointegration period, which is roughly the first six months. Not that at this point biological osseointegration was achieved. This takes up to one year or more, Dr. Nobre points out, but at this point in time the implants can withstand load. The second phase of maintenance starts with the insertion of the definitive prosthesis.
Dr. Nobre moves to the first phase of maintenance with receiving the patient from surgery, and highlights that we have the responsibility of delivering the patient to the prosthodontic department in good form for them to manufacture the definitive prosthesis. And so us to get to that goal, we need to achieve some short-term goals which are preventing infection, reduce patient discomfort, and induce healing of both hard and soft tissues. To do that, we separate very clearly between what is the patient's responsibility and what is the clinician’s responsibility because we provide a treatment warranty. Continuing with the patient's responsibility, let's start with this question: What is the right chemical product to aid the mechanical plaque control during this functional osseointegration period? We might think about chlorhexidine, for example, it's probably the chemical most studied with loads of scientific literature backing it up. While he would feel comfortable providing it to the patient, it may cause problems, if the patient not only looked for functional but also for esthetic rehabilitation – chlorhexidine has the side effect of leaving brown stains, which could cause the patient to stop using it. So, it will not be effective. We should not only bear the effectiveness in mind but also adverse effects and efficiency. What if we have the greatest product in the world, but the patient just can't afford it? Or if the patient does not see any advantage in paying for the product. It might be surprising, but some patients are more than able to invest thousands of euros in an implant rehabilitation, but when they are present with a gel or a toothpaste that is a little bit pricier, they complain about it. All of this had been considered when this protocol was built. This protocol and most things that we will hear about this protocol are all based on published science. Dr. Nobre continues by showing us a table with products and mentions, that this clinical trial was published in 2007. Amongst the products that were compared were also chlorhexidine and hyaluronic acid. Hyaluronic acid is a natural component which can absorb up to 50 times its molecular weight in water, which makes it a kind of a natural healing agent. The disadvantage is, if the patient smokes, it is not the right product, as the hyaluronic acid is degraded by nicotine. Also, the price is relatively high, and it is difficult to find outside of Europe. The next product Dr. Nobre discusses is Chitosan. Chitosan is an antibacterial and hemostatic agent, which is extracted from shellfish. So, if the patient is allergic to shellfish, this product cannot be used. The next product on the list is cetylpyridinium chloride which is an antibacterial of low price and relatively widely available, but it leaves stains like chlorhexidine. The final product on the list is triclosan, also an antibacterial of low price and easy to find, but some countries like the United States of America, have restricted the use of triclosan in, for example soap, because of its environmental impact. Dr. Nobre concludes that the selection of products depends on where we are in the world and which products are available to us. We can recommend all these products to the patients, but we need to make sure that the product is adapted to the patient and not the other way around. He continues his lecture by moving on to the responsibilities of the patient. During the first 10 days of maintenance, the patient brushes at least 2x per days with a post-operative toothbrush with very soft bristles and start massaging and applying one of the previously discussed chemicals and rinses the mouth with the same. Dr. Nobre explains that they avoid mixing different products to avoid any antagonistic effects. Between day 10 and 2 months, the routine continues, the brush is exchanged for a soft medium bristle toothbrush after one week, and they start to educate the patient to use other mechanical means of plaque removal. He points out that the recommendation of a water flosser at this time should be considered as the soft tissue is not yet healed. 2-4 months post-surgery, the patient is using a soft medium bristles toothbrush with a low abrasion dentifrice and other mechanical means of plaque removal. The self-care should be easy for the patient. What is the clinical responsibility, asks Dr. Nobre. He refers to a graph from Glauser et al. , showing on the left side the frequency analysis measured in Hertz, which he interprets as the force with which the bone grabs the implant between the brackets. The other axis shows the time in months. The study compares a machined implant surface with the TiUnite implant surface, and registered that at day 0, the day of surgery, the force with which the bone grabbed the implant was very high. But this is not the final anchorage of the implant. The primary anchorage at that day can be manipulated, for example, by under-preparation. This force goes down with time and reaches its low at 2-3 months and then increases again, reaching a plateau at 3-6 months. What does this mean for the maintenance? Dr. Nobre tells us to follow this curve by planning the dental hygiene appointments at day 0, 10 days, 2 months, 4 months, and 6 months. The other reason for this rhythm is to prepare the patient over 6 months and 5 appointments to get used to visit the clinic for maintenance and prevention, not because of pain. Especially patients with a history of periodontitis are not used to visit the clinic unless they are in pain. This period is a forming period for the long-term maintenance. What should these appointments cover? He shares with us the concept of the “hand”, a concept of 5 clinical indexes, including mobility, suppuration, plaque, bleeding, and probing. Epidemiologically, the four indexes mobility, suppuration, bleeding and probing of pocket depths have different sensitivities and specificities which help us to get a very close oversight and any problem that might occur is noticed early on. The main goal of the concept is a correct diagnosis as early as possible. Starting with the first index, the mobility, Dr. Nobre explains that by using, for example, a tweezer, he applies movement to the top of the abutment or implant. If mobility is detected, this means either the abutment is loose, or the implant is lost. Another simple test is testing for suppuration by finger pressure. If finger pressure is applied and suppuration is appearing. If suppuration is present, this may indicate a large infection. On the other side, if we don’t see suppuration, we should not rule out infection, we should finish the other tests first. The third test is the modified plaque index, developed by Mombelli et al. He explains in detail how to execute the test by inserting the periodontal probe 1mm into the sulcus and running a circle around the abutment or implant and then score in a scale from 0 to 3. No detection of plaque equal 0, 1 equal “I only saw plaque after the movement”, 2 represents that plaque was visible without movement and 3 equals plaque with food debris. He demonstrates the different scores with clinical examples.
Why are the modified plaque and bleeding index helpful? Dr. Nobre explains that they help us to transfer information objectively, as everyone knows the meaning of the indexes. The next and final point is probing of pocket depths. This is a controversial topic and there are two sides, one who probes and one who doesn’t probe. Dr. Nobre explains the key difference between probing natural teeth and probing implants: when probing natural teeth, we are pushing the fibers down, but when we probe an implant with too much pressure, we are breaking the mucosal seal. According to Dr. Nobre, not probing itself is the issue but probing incorrectly. Sometimes the first impression looks good, but after running the test this impression changes, he exemplifies this with a case. But how we probe correctly? By using a periodontal plastic probe, calibrated to 0.25 Newtons, which means 25 grams of force and evaluating on four points, no depths should be more than 4mm. There are two reasons for this value: First one being that below 4 mm the kind of bacteria developing are anaerobic bacteria. And second, because there is no tool that can clean without provoking significant damage below 4 mm. A water flosser could be used, direct at the implant with maximum pressure, but this will do much more than cleaning, it will cause trauma to the complex. Dr. Nobre shares that he likes to use calibrated probes, but they have been discontinued by the manufacturer. So, he started to calibrate himself and the team. He demonstrates how we can learn how to probe with the correct among of pressure by using way strips and a plastic probe. Another option is to use a precision scale and placing the fulcrum outside of the scale, press to reach 25 grams and train the muscle memory for this pressure.
What happens at the appointments? Dr. Nobre continues his lecture with the 10-day appointment, where they do an orthopantomography, if it wasn't performed on the day of surgery, and they take periapical radiographs to record base line bone levels, and take advantage of performing the Sheffield test, especially for All-on-4 cases. The prosthesis is removed, disinfected, and cleaned, and if the healing is ok, the sutures are removed. After this, the “hand” is performed with checks for mobility, suppuration, plaque, and bleeding, but no probing should be performed on day 10. Maybe hyaluronic acid is applied to the wound if the soft tissue healing is delayed. The abutments are polished with a rubber cup and chlorhexidine gel. The prosthetic is checked for fractures or loosening of components, and the patient is instructed not to overload. The surgical department checks the occlusion. At the 2 months appointment the same points are checked, including probing and at 4 months this is repeated. If the peri-apical radiographs are evaluated as ok, the patient is sent to the prosthodontic department for manufacturing of the final prosthesis. The next appointment follows at 6 months, and this also marks the end of the first phase of maintenance and start of the second phase. How do we care for the prosthesis? Ultrasonic tips can help us to remove plaque off the prosthesis, an air flow device with bicarbonate powder can also be used, as it will remove food debris, plaque, calculus, and stains from the denture. In terms of using instruments on the implants, Dr. Nobre recommends using an ultrasonic scaler with a plastic tip. Material that gets in contact with implants should have three characteristics: firstly, is to be plastic, secondly is to be thin enough to penetrate the sulcus, and thirdly is to be able to be sterilized and reused again otherwise the investment is going to be really, really high. The abutments can be cleaned with a chlorhexidine gel and a rubber cup in, for example, circular motion. We need to ensure that the complete peri-implant sulcus is disinfected and cleaned. Also, here the air flow can be used with glycine powder or erythritol powder at low speed and water and circular movement. He continues to demonstrate this workflow with a clinical case. He challenges us to change the mindset from “everything is ok” to “there is something there” and that we should always be alert and use all the tools available to us.
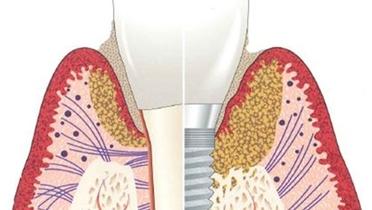
The second phase of maintenance is also separated into the responsibilities of the patient and the clinical responsibilities. One of the responsibilities of the patient is to not miss a maintenance appointment. The clinical and radiographic diagnosis should always be done first before commenting on the status to the patient. The individualized hygiene instructions should be reviewed, and the patient should be motivated, after that we move to the instrumentation. This is followed by the planning of the next visit based on the risk profile of the patient. When performing the radiographic evaluation, Dr. Nobre points out that the quantity and quality need to be considered. For the first 5 years a radiograph is taken annually, then every 2 years. Exceptions are important landmarks such as 10 years, 15, 20 and 25 years. With these the marginal bone loss is evaluated based on quantity and quality. Quality deals with the angle between bone and implant: if we have more than 60 degrees between bone and implant in an angle, then we have horizontal bone loss, a better prognosis because the soft tissues have the tendency to accompany that marginal bone loss. On the other hand, if we have an angle of less than 60 degrees between implant and bone, then you have vertical bone loss, a not so good prognosis because usually pockets are formed. In terms of quantity, it all come down to the point of occurrence, highlights Dr. Nobre. Is it the bond level on the coronal third, where we want it? Is it on the middle third, where we are already afraid because there is a limited prognosis for this implant, or is it on the apical third where basically here the implant is a zombie? We need to keep the diagnosis for the long-term, evaluate it regularly, observe it and have the occlusion checked at least once a year. He mentions that they take out the prosthesis out once every 3 years to confirm the tightening of the prosthetic components. Sometimes the prosthesis hinders a correct probing, it is advantageous to do it when it is removed. It will be checked for fractures or chips, depending on the material. But all of this depends on the kind of patient that we have. Dr. Nobre reminds us to evaluate the motivation of the patient as this is crucial, and they are responsible for maintaining their health. We should never give up on a patient, even if we must repeat the same point repeatedly.
Next, Dr. Nobre explains the effects of instruments on the restoration or implant. Polishing can be done, using a rubber cup and low abrasive polishing paste. The RDA of the paste should be below 10. Superfloss can be used around the prosthesis. He continues to show us the effects of curettes on the implant or abutment surface. He compares three different types of curettes and demonstrates the advantages and disadvantages of each. He concludes that the ultrasonic scaler is a better solution, if not used with a stainless-steel tip! But also, plastic instruments can cause problems, for example if they are too soft and the tip is damaged. This could lead to plastic debris in the peri-implant sulcus. He recommends using instruments with peek coating, peek is a high resistant polymer which he has made good experiences with. Dr. Nobre continues by showing us the effects an air flow can have on titanium surfaces when used with bicarbonate powder. Air flow should only be used in this context with glycine or erythritol powder to go below the mucosal margin. Moving to the individualized hygiene instructions for the patient, we learn that the toothbrush should be adapted to the patient and that we should instruct the patient how to clean the interface between mucosa and prosthesis or crown. An alternative can be electronic toothbrushes as they help to avoid too much pressure. Especially patient with a full-arch rehabilitation can benefit from these brushes as they tend to lose their receptive sensitivity. When it comes to the interface, we need to evaluate the size of it and select the right plaque removal tool. A small interface will be limited the options but will naturally have less plaque accumulation. A large interface can be cleaned with almost any device but has the disadvantage that it will get more plaque accumulation. A water flosser can help with small interfaces, as it removes food debris and immature plaque. On the other side, the patient needs to use it meticulously, and if they stop using it and the plaque matures, the water flosser will not be able to remove it.
Dr. Nobre moves on to the topic of risk factors and points out that the major risk factor for late implant failure is peri-implant pathology. He shares the strategy they have established, based on 3 steps: measure the risk, manage the risk, and communicate the risk to the patients, to make them accountable. The strategy shared is built on scientific literature, published in peer-reviewed journals with a high impact factor. A lot of variables have been evaluated through multivariable analysis and a model for peri-implant pathology was established. The selected variables are these ones, from history of periodontitis, bacterial plaque, the bone level, smoking habits, bleeding, the type of material used on the restorations. If there are prosthetic loosening or passive misfit issues, the proximity of other teeth or implants that function like a protection biomechanically, in the presence of plaque there will be no protection anymore, it will function like a bacteria reservoir. Therefore, it's nice to know the odds ratios to see how many times the chance increases in determined characteristics. For example, a patient with plaque has 3.6 increased chances of having peri-implant pathology compared to a patient without plaque, according to Dr. Nobre. But with the odds ratios, we cannot estimate anything, what we can do to estimate is using the beta values. He indicates that the model has an accuracy of 94.3% of the cases that had and didn't have the incidence of the disease. The calculation was made easier for us as it was transformed into a risk score based on the presence or absence of the variables, and then we have four levels: green level, low risk, with less than two points; moderate risk, with two to four points; high risk at five to seven points; very high risk with more than seven points. When using the scientifically validated calculation we will have a tool that will get right 85.8% of the cases, four years in advance. Moving to the second part of the strategy, the management of the risk, meaning which risk profiles do we have? The first implication is recall, for low-risk patients, green patients, a six-month recall; for yellow patients, moderate risk, a four-month recall; for high-risk patient a three-month recall, and for very high-risk patients a two-month recall rhythm. But there are other implications, such as patient education and motivation and if the problem is the prosthetic design, we should change it. And the third step is to communicate the risk to the patient, and we must do this preferably before something happened. We must get the patient accountable for their own health status, Dr. Nobre emphasizes. To make this easier for us, he and his colleagues have donated the risk assessment tool to FOR and we can find it on the website. He shares that he uses the tool with patients, who’s recall rhythm must be adapted due presence of risk factors. This helps to avoid misunderstandings in terms of paying for additional appointments which are not required, in the mind of the patient. He fills in the tool together with the patient and presents them with the result. After filling in the short questionnaire and clicking on “Finish”, the tool will provide us with a risk profile and suggest a recall schedule. We can download the results and add them to the patient file. What about the prognosis? We measure the risk in implants that don't have the disease, what is the probability of implants without peri-implant pathology to develop it? In a study with 240 patients with peri-implant disease that were collected from an epidemiological surveillance study with over 22,000 patients, and randomly selected half of the sample to derivate the model and half the sample to validate the model. They investigated potential prognostic predictors, and as an end point, they would say that an unfavorable prognosis is either if we lose the implant, if we have progressive marginal bone loss, or if we have a prevalence or aggravation of peri-implant pockets. And the time to evaluate this was one year after the diagnosis was performed. The study was published 2019, a lot of variables were studied, some of them on the demographic aspect, some of them on habits, some of them with factors related to the rehabilitation, others with the follow-up time. Out of all the variables five were selected, summarized in a tool that will get an accuracy, one year advance, of 76% of the cases. In the coming weeks, this tool will also be available for us on FOR.org. But Dr. Nobre leaves us with a warning, the prognostic score should not be taken for the decision of keeping the implant or removing the implant because that was not what it was designed for. This tool should be used as a clinical aid to prepare us for what is to come. To indicates this, he shares a clinical case and explains how to use the results for clinical practice. His advice to achieve excellence in the long-term is to approach it step by step, appointment by appointment and keeping the focus on the present and immediate future.
References
[1] de Araújo Nobre M, Cintra N, Maló P. Peri-implant maintenance of immediate function implants: a pilot study comparing hyaluronic acid and chlorhexidine. Int J Dent Hyg. 2007 May;5(2):87-94. doi: 10.1111/j.1601-5037.2007.00239.x. PMID: 17461960.
[2] Glauser, R. & Portmann, M. & Ruhstaller, P. & Lundgren, A.K. & Hammerle, Christoph & Gottlow, Jan. (2001). Stability measurements of immediately loaded machined and oxidized implants in the posterior maxilla. A comparative clinical study using resonance frequency analysis. Appl Osseointegration Res. 2. 27-29.
[3] Silverstein LH, Kurtzman GM. Oral hygiene and maintenance of dental implants. Dent Today. 2006 Mar;25(3):70-5; quiz 75. PMID: 16617795.
[4] de Araújo Nobre M, Mano Azul A, Rocha E, Maló P. Risk factors of peri-implant pathology. Eur J Oral Sci. 2015 Jun;123(3):131-9. doi: 10.1111/eos.12185. Epub 2015 Apr 20. PMID: 25894059.
[5] de Araújo Nobre M, Mano Azul A, Rocha E, Maló P, Salvado F. Attributable fractions, modifiable risk factors and risk stratification using a risk score for peri-implant pathology. J Prosthodont Res. 2017 Jan;61(1):43-53. doi: 10.1016/j.jpor.2016.03.004. Epub 2016 Mar 29. PMID: 27032718.
[6] de Araújo Nobre M, Salvado F, Nogueira P, Rocha E, Ilg P, Maló P. A Peri-Implant Disease Risk Score for Patients with Dental Implants: Validation and the Influence of the Interval between Maintenance Appointments. J Clin Med. 2019 Feb 17;8(2):252. doi: 10.3390/jcm8020252. PMID: 30781553; PMCID: PMC6406564.
[7] de Araújo Nobre, M.; Salvado, F.; Nogueira, P.; Rocha, E.; Ilg, P.; Maló, P. A Prognostic Model for the Outcome of Nobel Biocare Dental Implants with Peri-Implant Disease after One Year. J. Clin. Med. 2019, 8, 1352. https://doi.org/10.3390/jcm8091352