N1 implant in aesthetic area: The digital approach to surgical and prosthetic rehabilitation
The patient is a 62-year-old woman who presented in good general health. She reported no history of systemic disease, no allergies, and was not taking any long-term medication. Her medical history was thoroughly reviewed, and no contraindications for oral surgery or implant placement were identified. From a general health perspective, the patient was considered to be in excellent condition for surgical and prosthetic treatment.
In terms of dental history, the patient maintained regular dental check-ups and demonstrated satisfactory oral hygiene habits. She did not present with any generalized oral disease or periodontal problems. Apart from the current clinical situation, she had no history of significant dental complications. This background created an ideal baseline for treatment planning, as systemic and oral risk factors were minimal, and the patient showed strong motivation for a comprehensive and esthetic solution.
Evaluation & Diagnosis
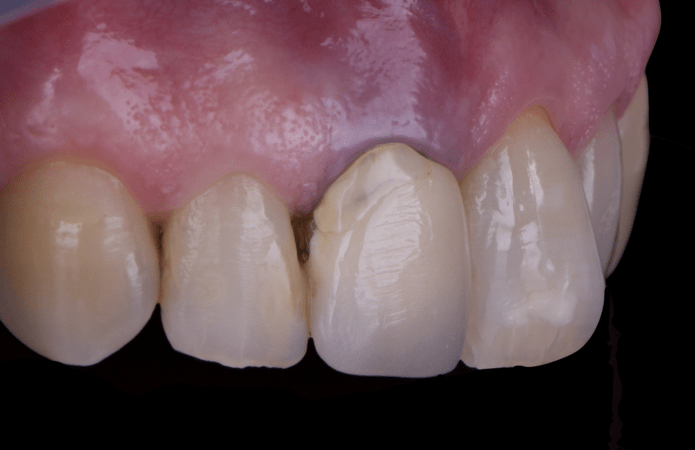
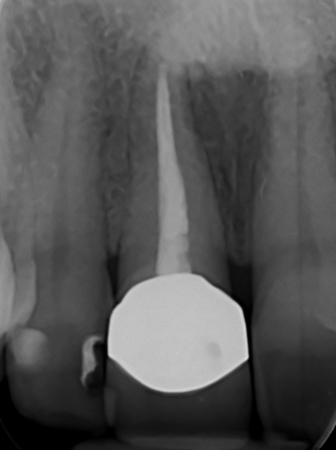
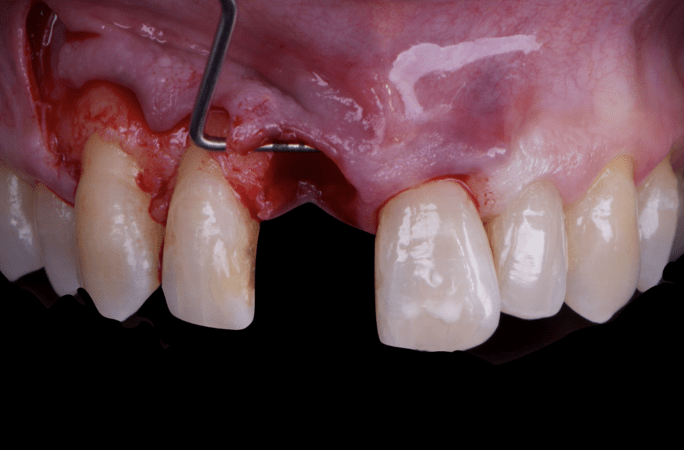
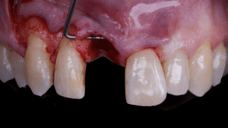
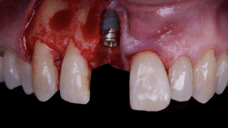
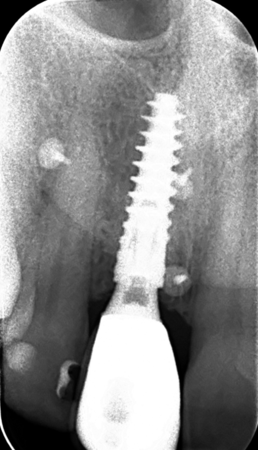
The main issue involved the upper right central incisor (tooth 1.1), which was devitalized and presented recurrent abscesses. Clinical and radiographic evaluation confirmed the presence of buccal bone wall resorption, leading to a significant defect in the alveolar ridge. This condition compromised both the hard tissue and the surrounding soft tissue, posing a challenge for achieving long-term stability and esthetic success in the anterior maxilla.
Due to the tooth’s location in the esthetic zone, the resorption and recurrent infections had a direct impact on the patient’s smile and overall confidence. She expressed dissatisfaction with the appearance of the affected tooth and emphasized the importance of restoring function and esthetics quickly. The clinical presentation highlighted the need for a treatment plan that combined immediate implant placement with simultaneous hard and soft tissue management to address the complex requirements of this case.
Progress & Completion
The patient underwent a thorough risk assessment to evaluate systemic, local, and esthetic considerations. As she had no systemic diseases and maintained good oral hygiene, the overall medical risk was low. Locally, the main risk factors included the compromised buccal bone wall, the presence of infection, and the esthetic sensitivity of the anterior maxilla. These conditions required careful planning to ensure that both hard and soft tissues could be regenerated and stabilized around the implant.
From a psychological and functional perspective, the patient expressed clear expectations: she desired a fixed solution, an immediate provisional to avoid any removable prosthesis, and a final result that would be indistinguishable from her natural dentition. Managing these expectations was a critical component of the treatment plan, as immediate implant placement with provisionalization would allow her to maintain confidence and comfort throughout the process.
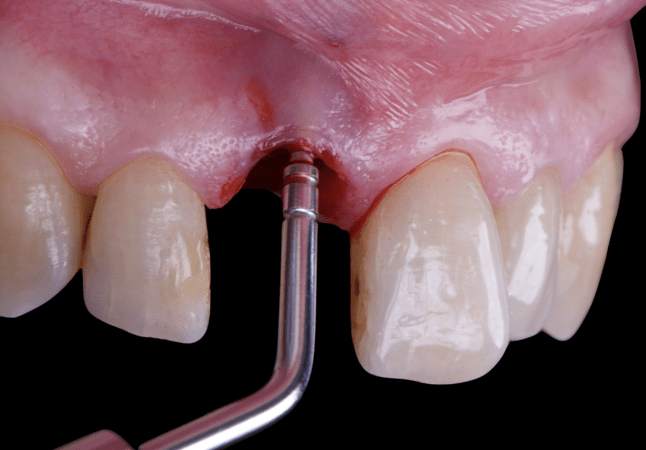
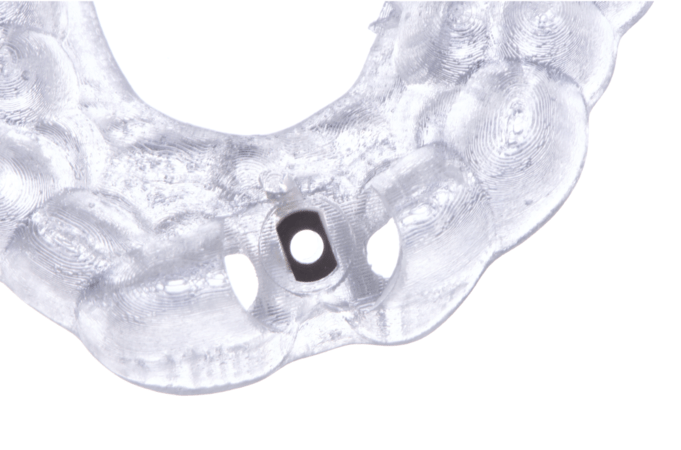
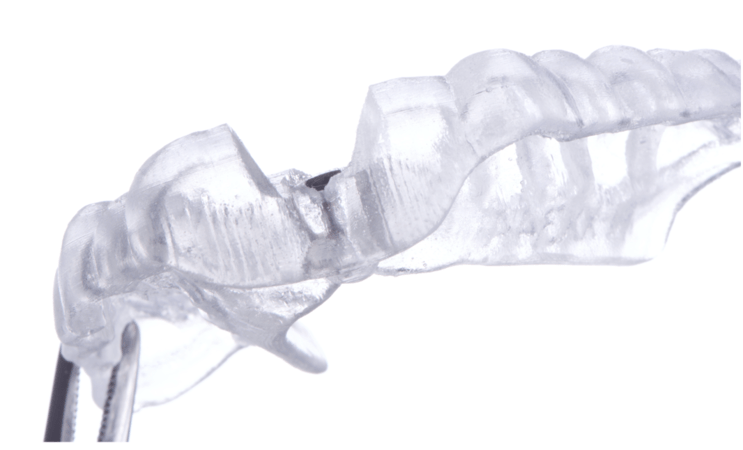
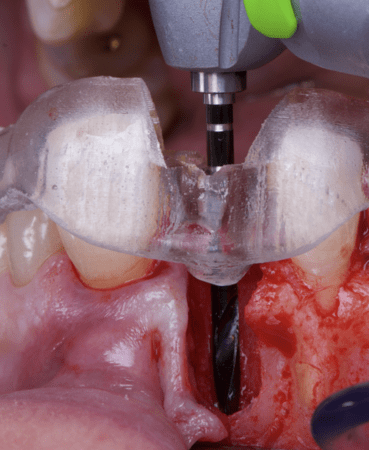
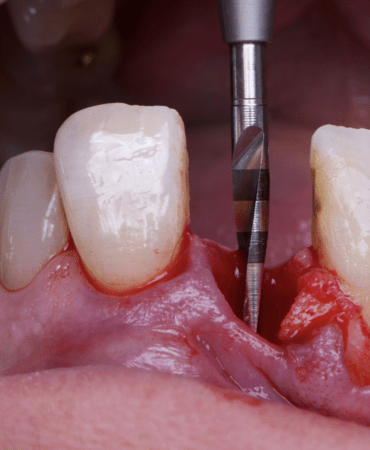
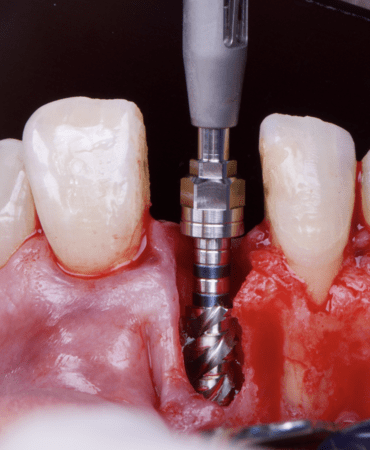
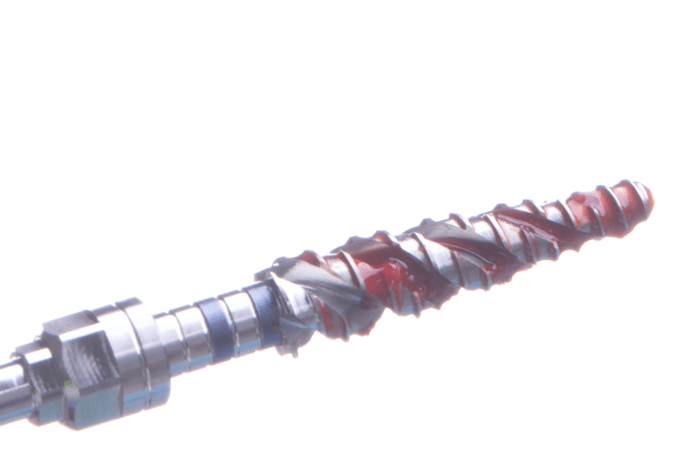
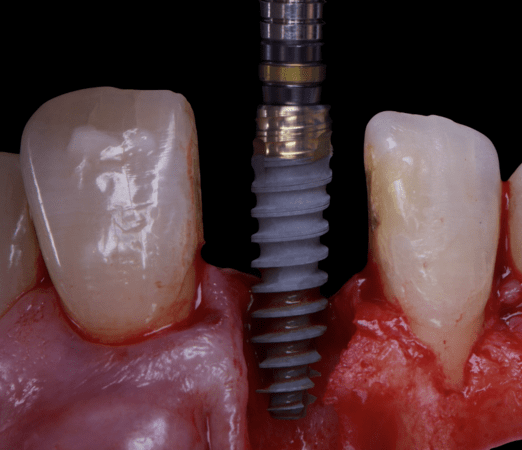
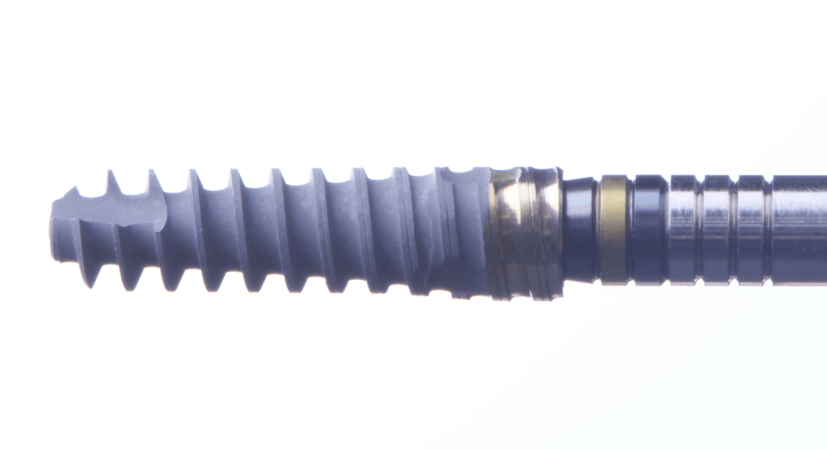
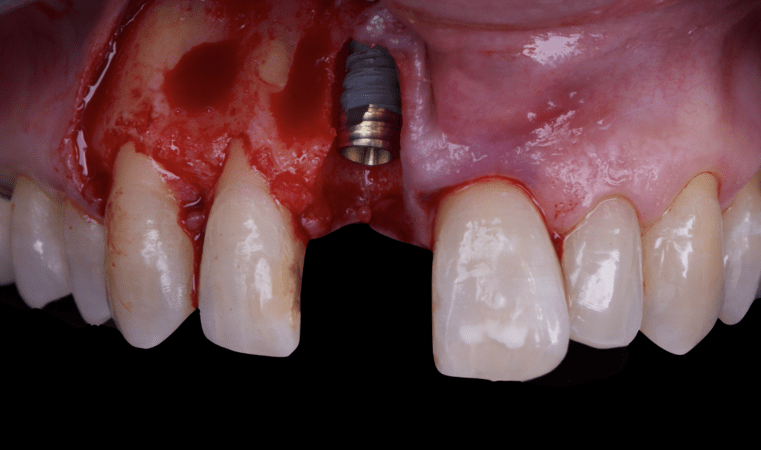
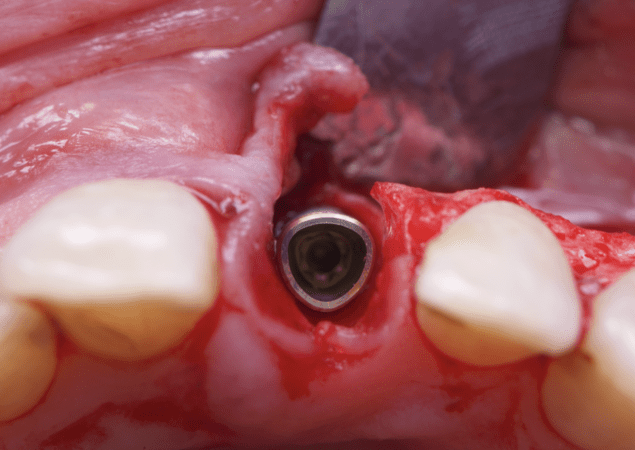
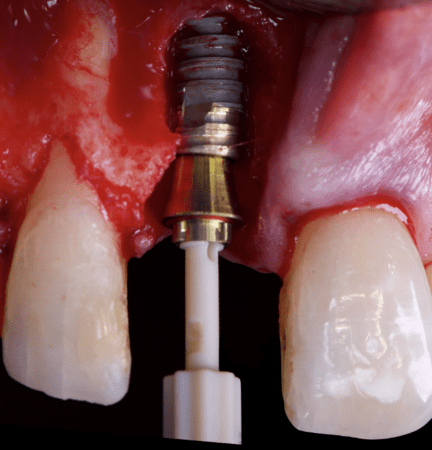
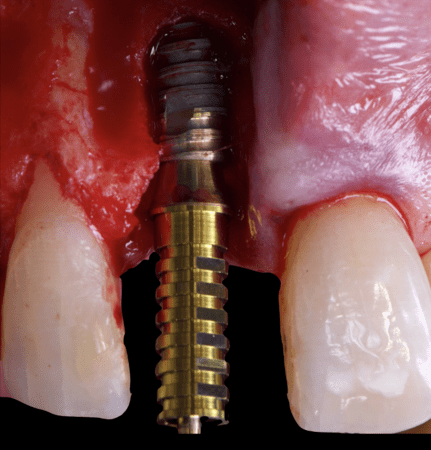
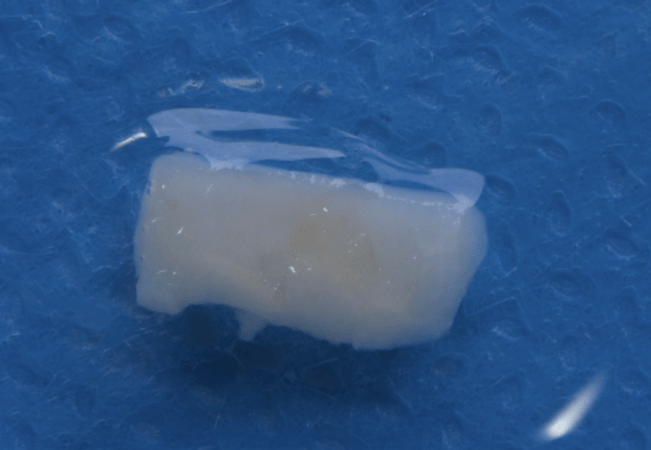
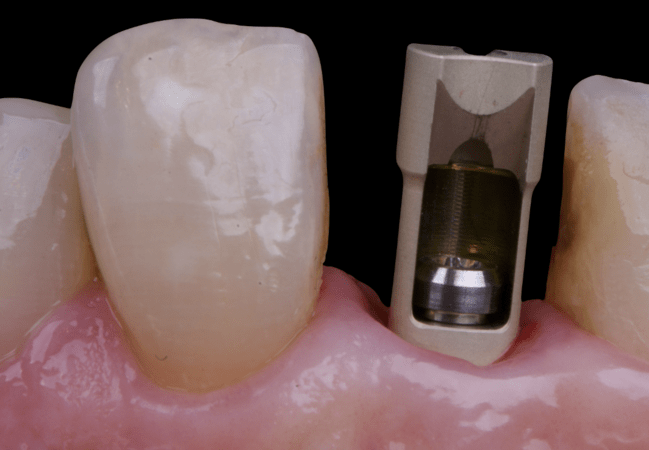
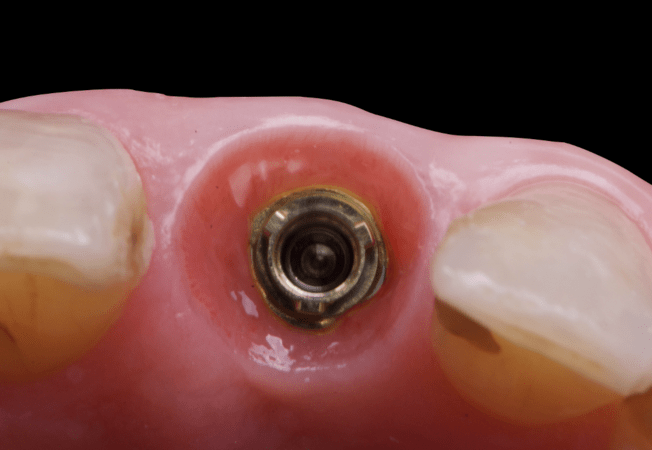
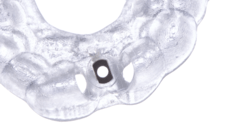
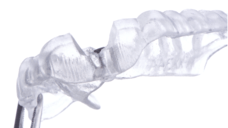
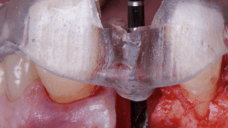
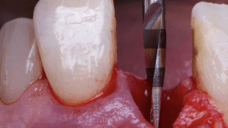
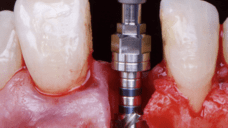
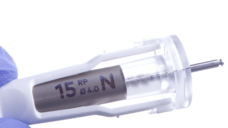
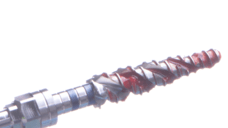
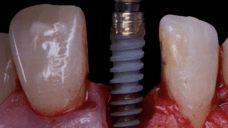
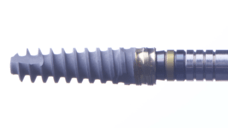
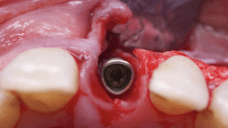
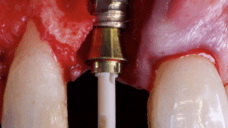
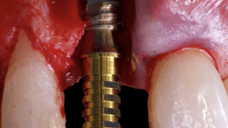
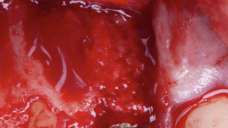
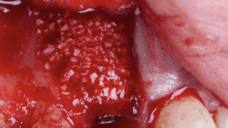
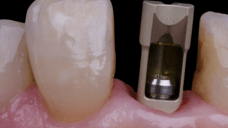
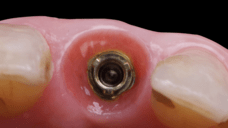
The surgical protocol began with the atraumatic extraction of tooth 1.1 to preserve as much of the alveolar socket as possible. Immediately following extraction, an N1 implant was placed into the socket using a guided surgical approach to ensure ideal three-dimensional positioning. The “one abutment one time” technique was applied to minimize soft tissue manipulation during the healing phase, which is particularly important in esthetic areas.
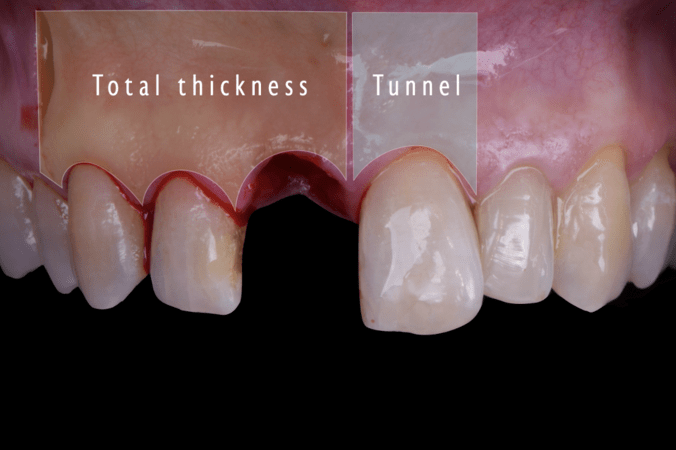
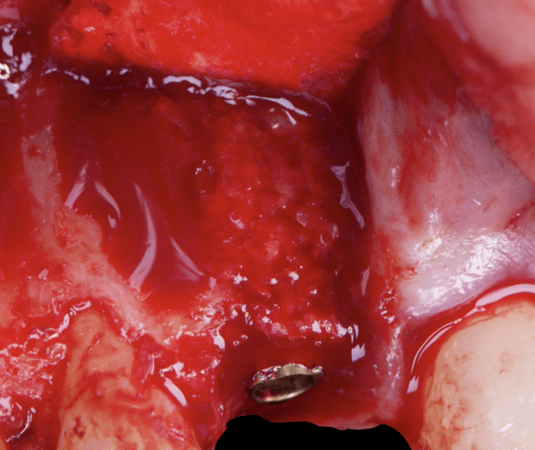
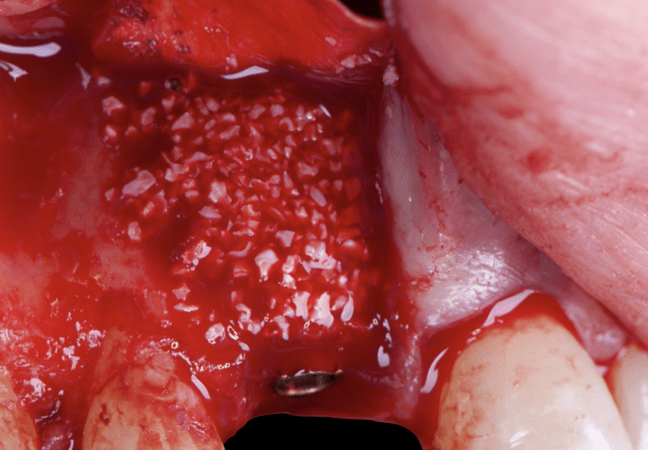
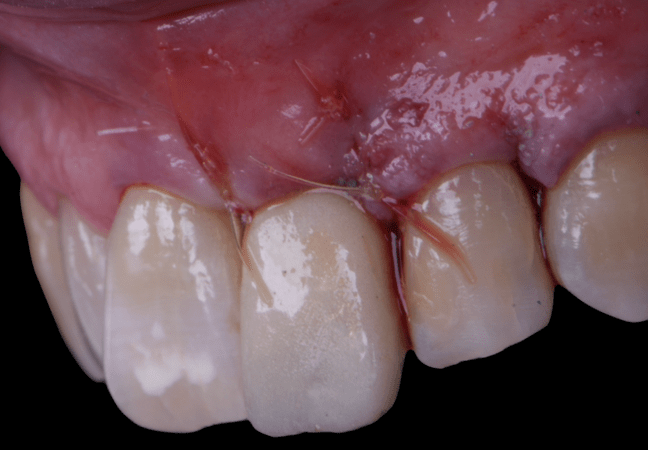
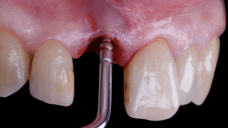
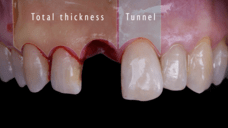
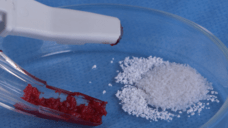
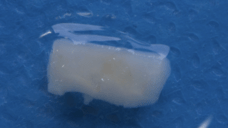
Given the significant buccal defect, guided bone regeneration (GBR) was performed simultaneously. A mixture of autologous bone and creos™ xenogain™ was applied to the defect and covered with a resorbable creos™ membrane to restore ridge width and support the buccal contour. In addition, a connective tissue graft was harvested and placed in the vestibular region to increase the thickness of keratinized mucosa. This combined approach addressed both hard and soft tissue deficiencies, providing the biological foundation for a stable and esthetic outcome.
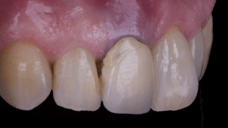
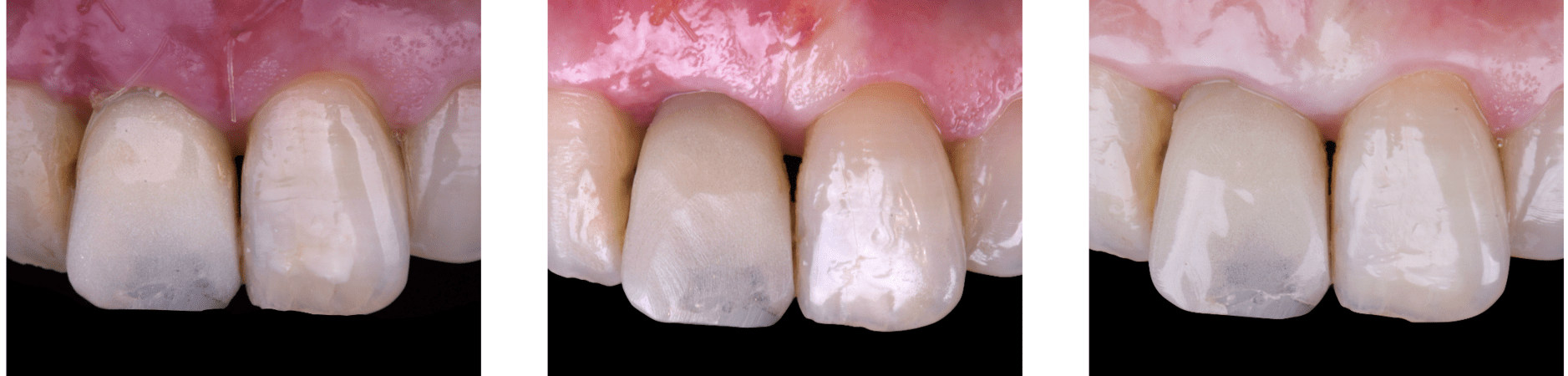
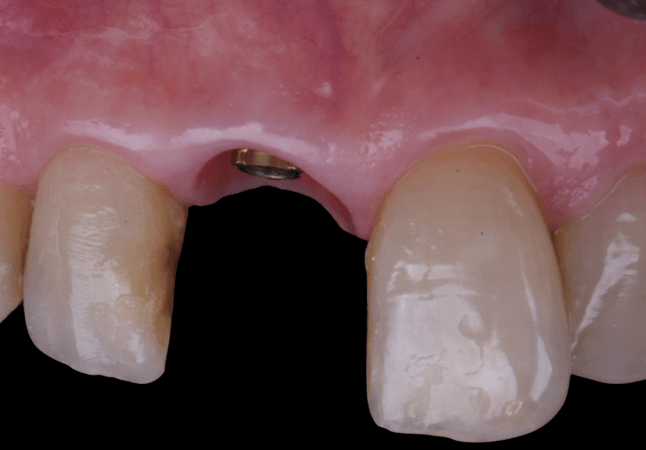
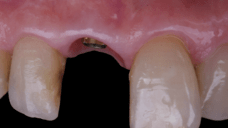
On the same day as the surgery, an immediate-load provisional crown was delivered. This restoration was fabricated in acrylic resin and screw-retained on the implant, following the “one abutment one time” principle. The provisional crown was carefully adjusted to avoid occlusal loading while supporting the peri-implant soft tissue architecture during the healing phase.
The provisional not only satisfied the patient’s functional and esthetic demands but also played a key role in shaping the emergence profile and conditioning the gingival margin. By providing a provisional solution immediately, the patient was able to leave the clinic with a natural-looking smile, avoiding any psychological or social impact associated with tooth loss in the anterior maxilla.
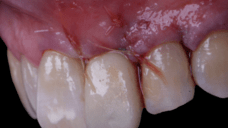
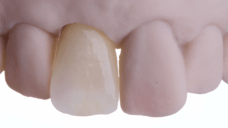
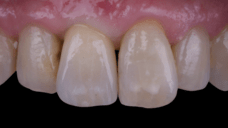
After an appropriate healing period, the definitive prosthesis was planned and delivered. A screw-retained zirconia crown was fabricated to ensure long-term durability, optimal esthetics, and retrievability. Zirconia was selected for its mechanical strength and excellent esthetic properties, blending seamlessly with the adjacent natural dentition in both form and color.
The final crown was designed to maintain the gingival architecture that had been shaped by the provisional. Special attention was paid to the emergence profile, contact points, and translucency to achieve harmony with the patient’s smile. The definitive restoration provided functional stability and esthetic integration, fulfilling the patient’s expectations for a fixed and natural solution.
Follow-up & Outcome
This case demonstrates the benefits of combining immediate implant placement with simultaneous guided bone regeneration and connective tissue grafting in a high-esthetic area. The use of the N1 system and the “one abutment one time” protocol facilitated predictable healing and minimized disturbance of peri-implant tissues. Immediate provisionalization contributed significantly to soft tissue shaping and patient satisfaction throughout the process.
Key learnings include the importance of careful planning when treating cases with buccal bone wall resorption in the anterior maxilla. The integration of advanced biomaterials, such as creos™ xenogain™ and membranes, along with soft tissue augmentation techniques, ensures stability of both hard and soft tissues. This case reinforces that implant treatment in esthetic zones can achieve excellent outcomes when biological and prosthetic principles are applied in harmony.