Maxilla anterior rehabilitation of hopeless incisor
Treatment began with a comprehensive analysis of the patient's dento-facial characteristics, guiding the selection of appropriate tooth shapes and sizes. Following patient approval of the proposed esthetic project, teeth 12, 11, and 21 were extracted. After socket healing, a CBCT scan was performed to evaluate bone volume, revealing horizontal resorption that was insufficient for implant placement.
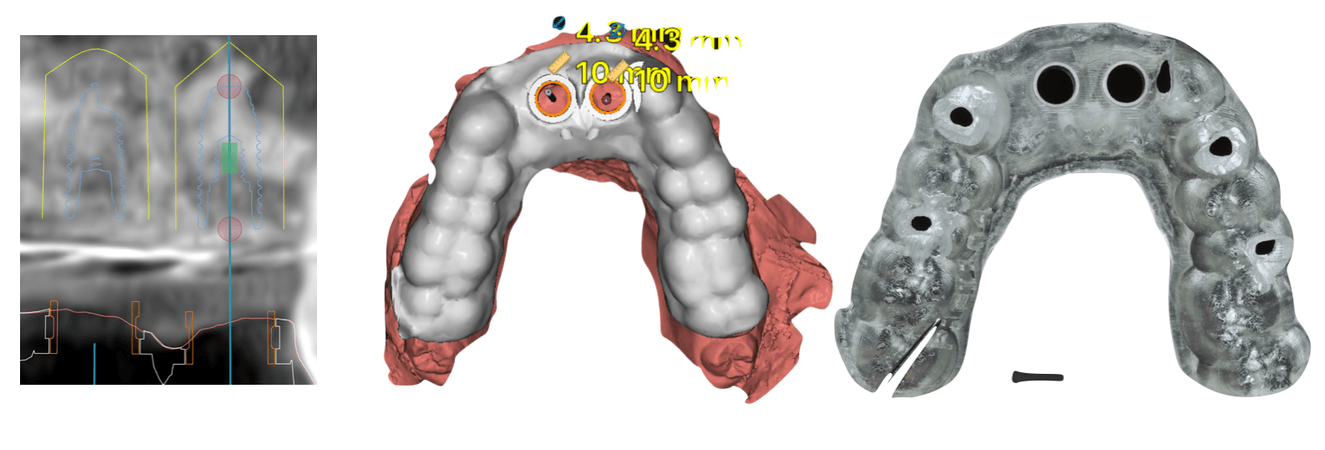
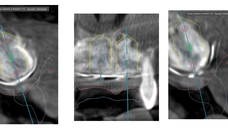
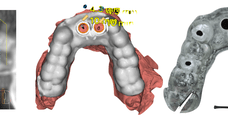
To address this, guided bone regeneration (GBR) was carried out using a combination of xenogenic and allogenic biomaterials, stabilized with a titanium-reinforced PTFE membrane. Nine months post-regeneration, a follow-up CBCT was aligned with a maxillary STL impression, enabling digital planning of implant placement using DTX software in accordance with the initial virtual design.
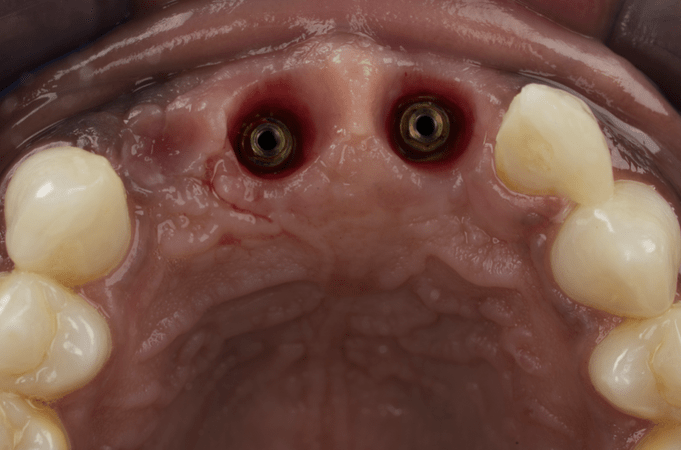
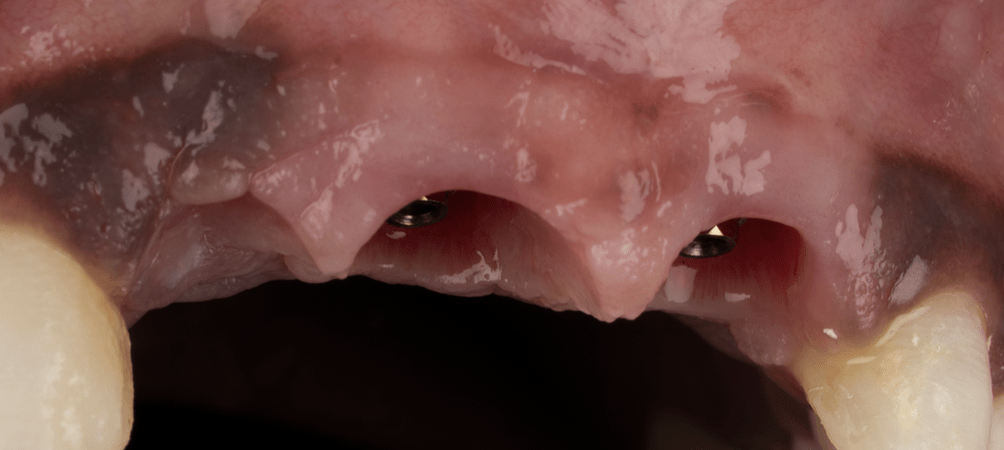
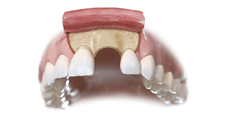
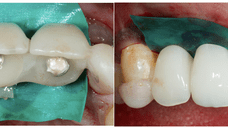
Implants were planned for positions 11 and 21, with a cantilever extension for tooth 12. Fully guided surgery was performed, and after successful osseointegration, a provisional bridge was placed to shape the soft tissue emergence profile. This customized profile was captured via a precise digital impression and sent to the dental laboratory.
The final prosthesis—a stratified zirconia bridge—was milled and torqued onto multi-unit abutments at 15 N·cm. The patient is currently under routine follow-up every six months.
Evaluation & Diagnosis
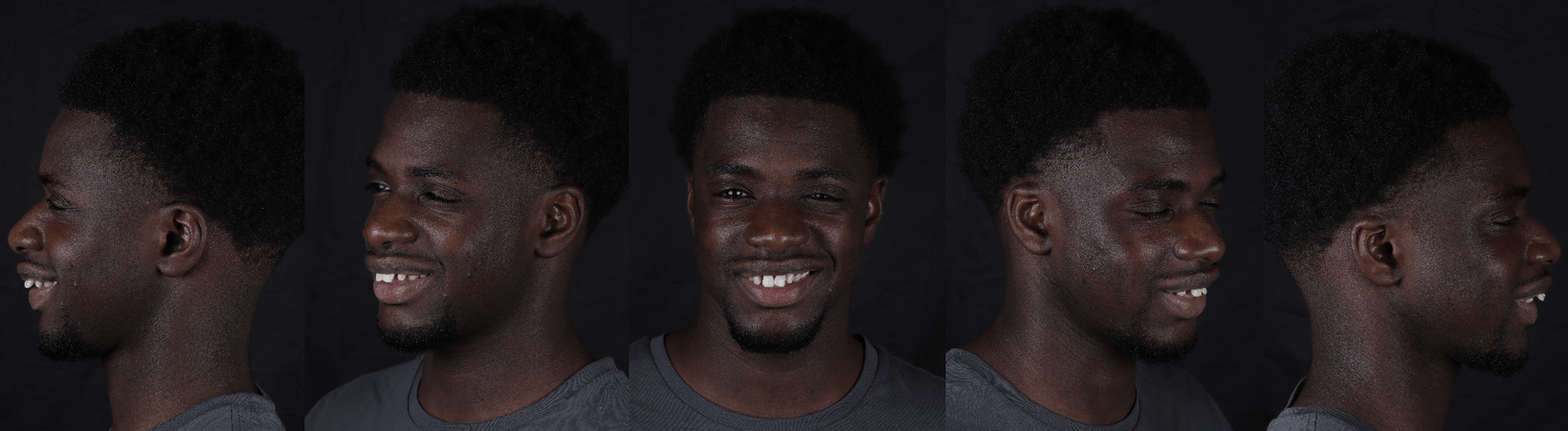
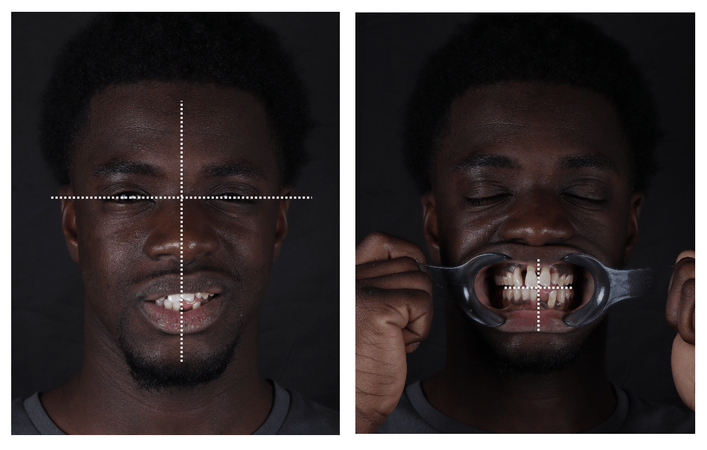
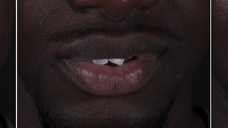
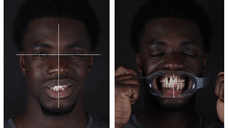
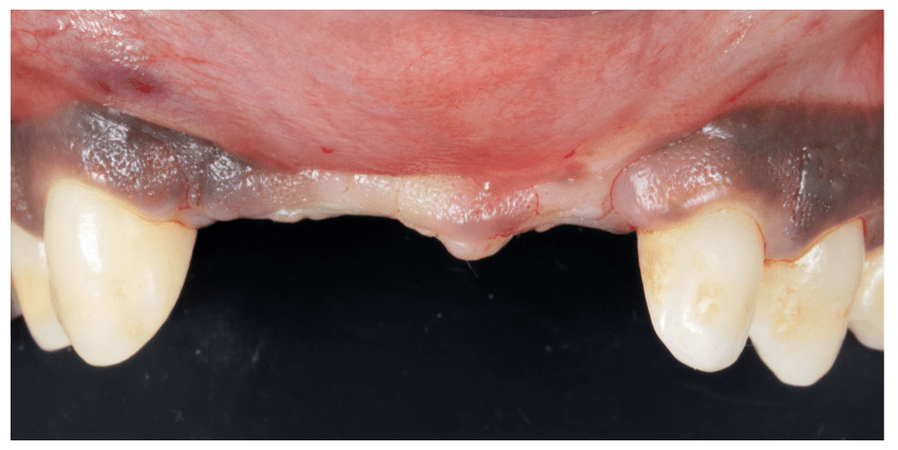
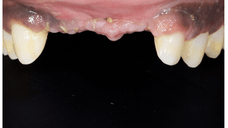
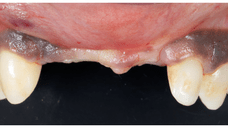
The patient first presented with aesthetic concerns regarding the maxillary anterior teeth. A comprehensive dento-facial analysis was conducted, including photographic documentation, intraoral scanning, and facial evaluation to understand the harmony between teeth, lips, and facial structures. Special attention was paid to midline orientation, incisal display at rest and during smiling, and gingival symmetry.
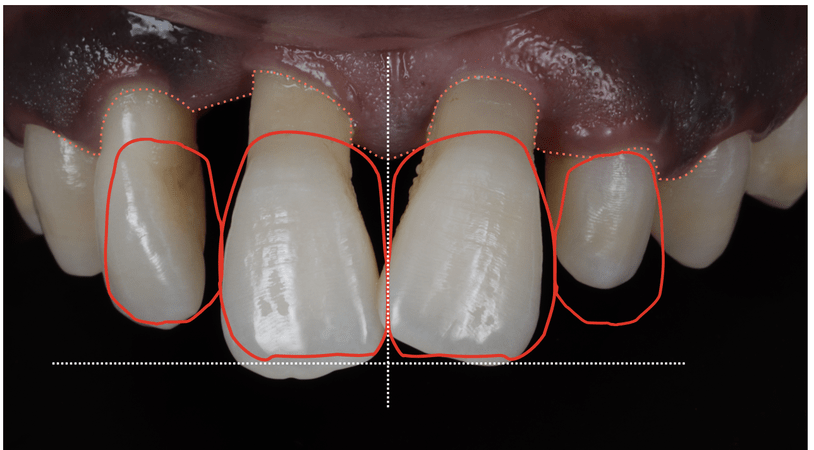
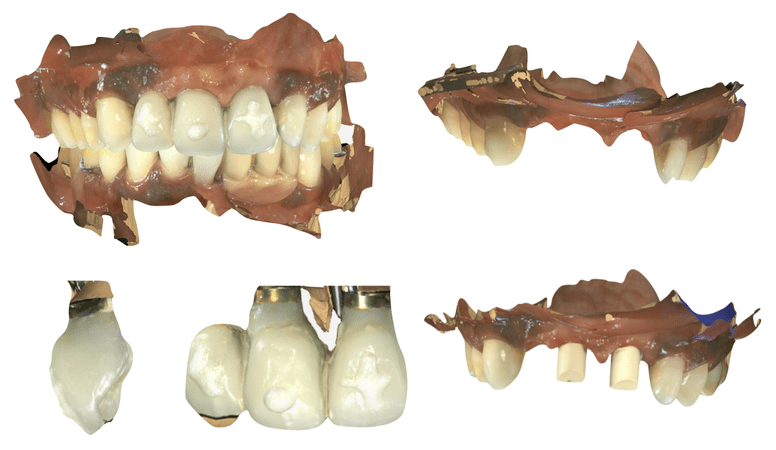
Various tooth shapes and sizes were discussed with the patient using diagnostic wax-ups and digital mock-ups. These tools allowed both the clinician and the patient to visualize the anticipated outcome, ensuring that expectations were aligned before proceeding with any irreversible procedures. The chosen design aimed for a natural aesthetic that respected the patient's facial proportions.
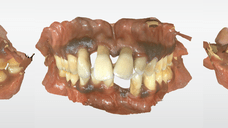
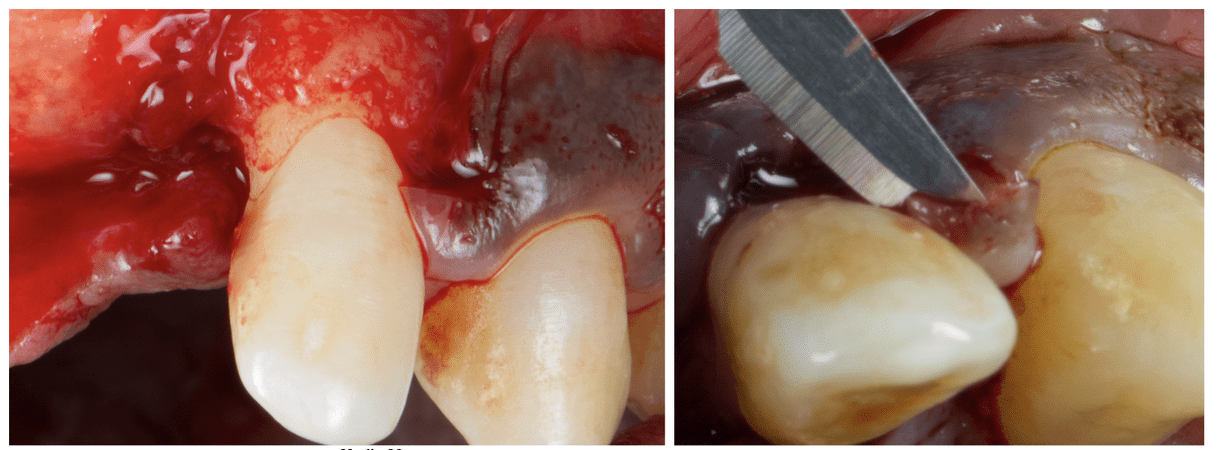
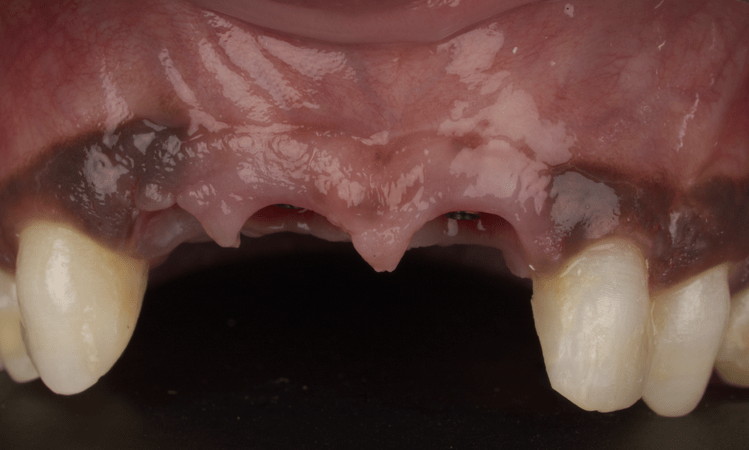
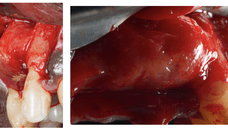
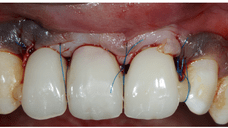
Following approval of the aesthetic project, clinical and radiographic examinations confirmed the poor prognosis of teeth 12, 11, and 21. The teeth were deemed unrestorable due to periodontal and endodontic complications, making extraction the only viable option. The treatment plan included extraction followed by guided bone regeneration to allow for future implant-supported rehabilitation.
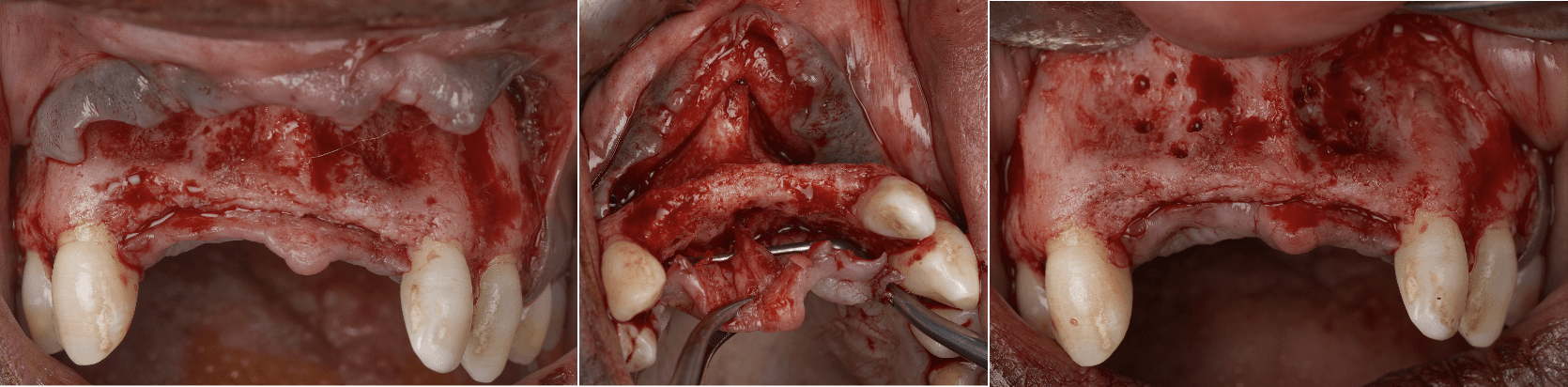
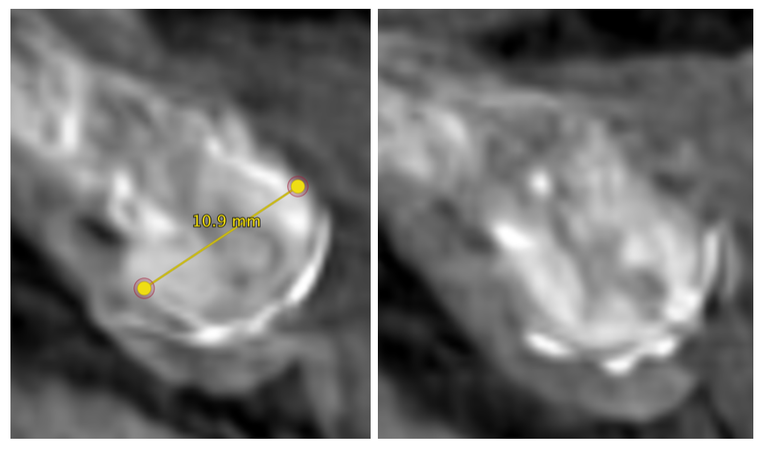
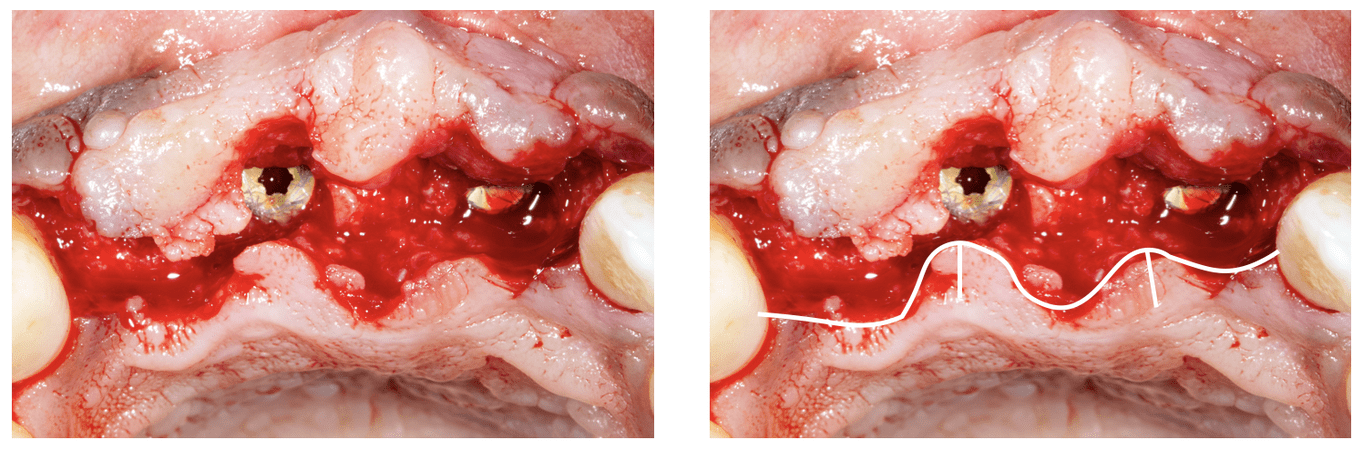
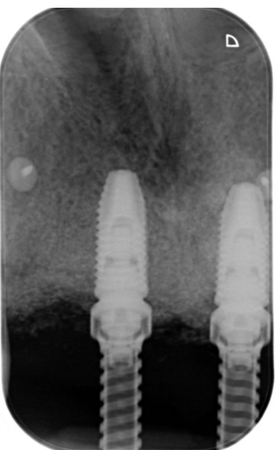
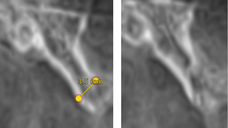
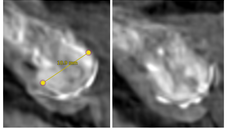
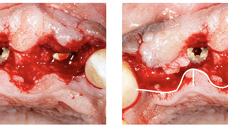
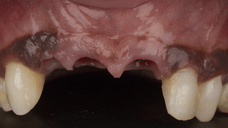
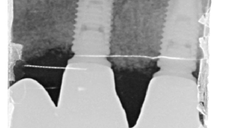
After atraumatic extraction of teeth 12, 11, and 21, a healing period was observed to allow soft tissue closure and initial bone remodeling. Once the sockets healed, a cone beam computed tomography (CBCT) scan was performed. The imaging revealed significant horizontal bone resorption in the anterior maxilla, making immediate implant placement unfeasible without prior bone augmentation.
Progress & Completion
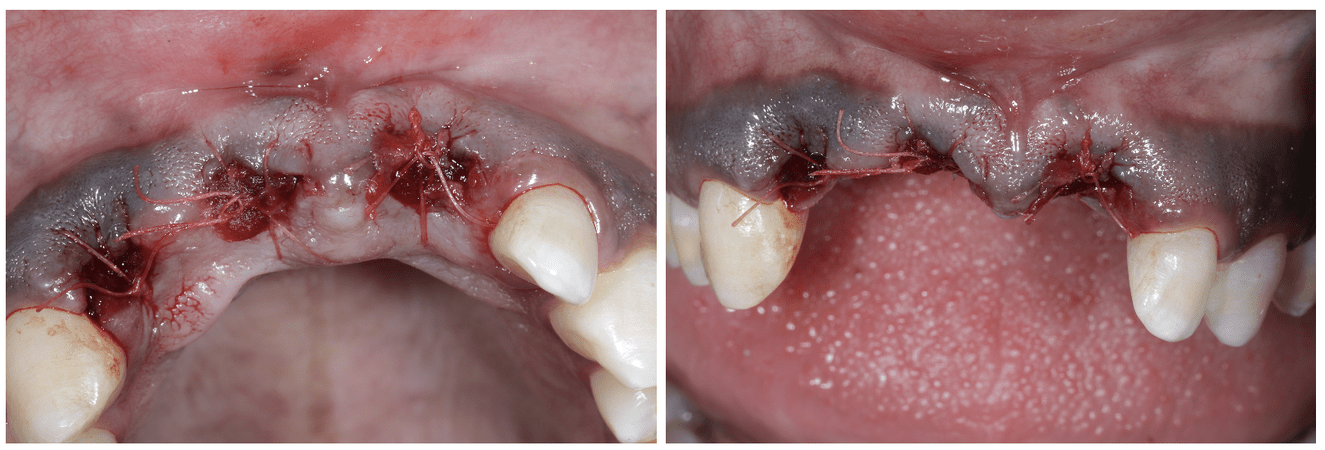
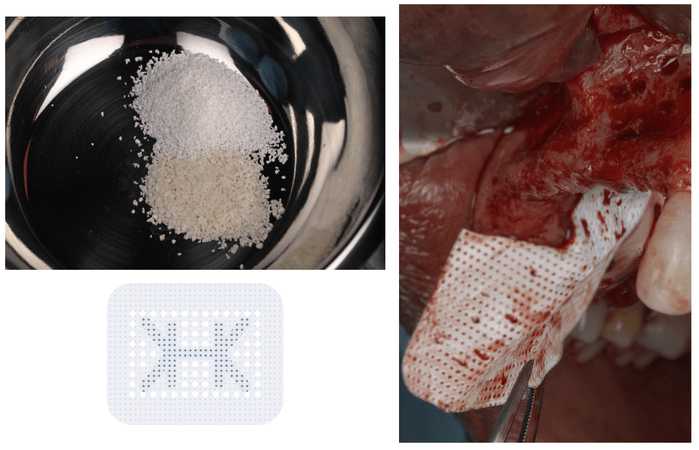
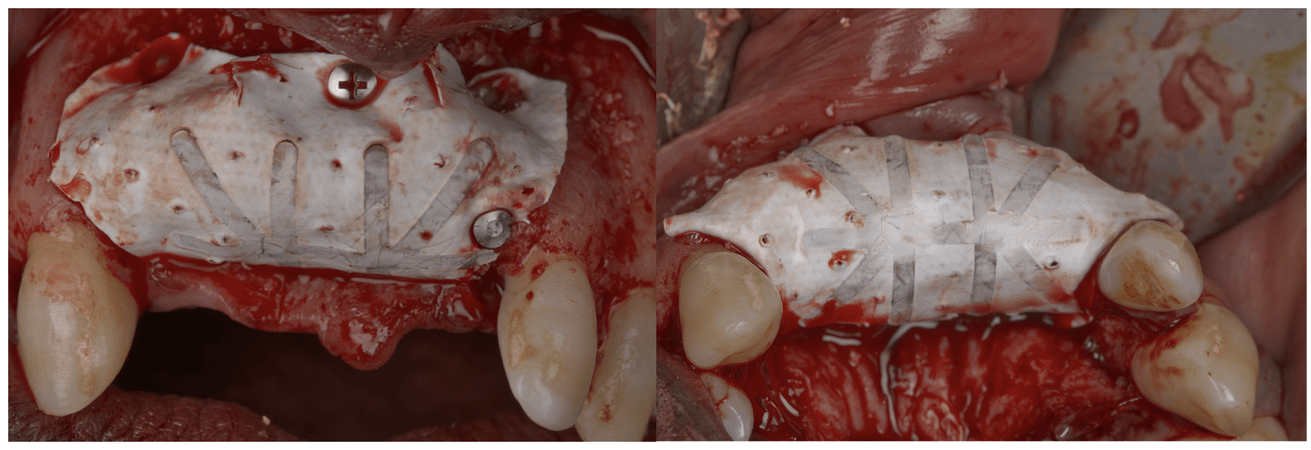
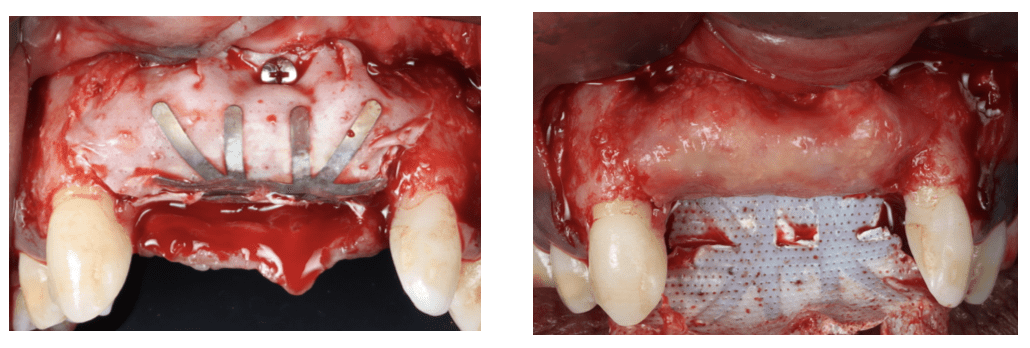
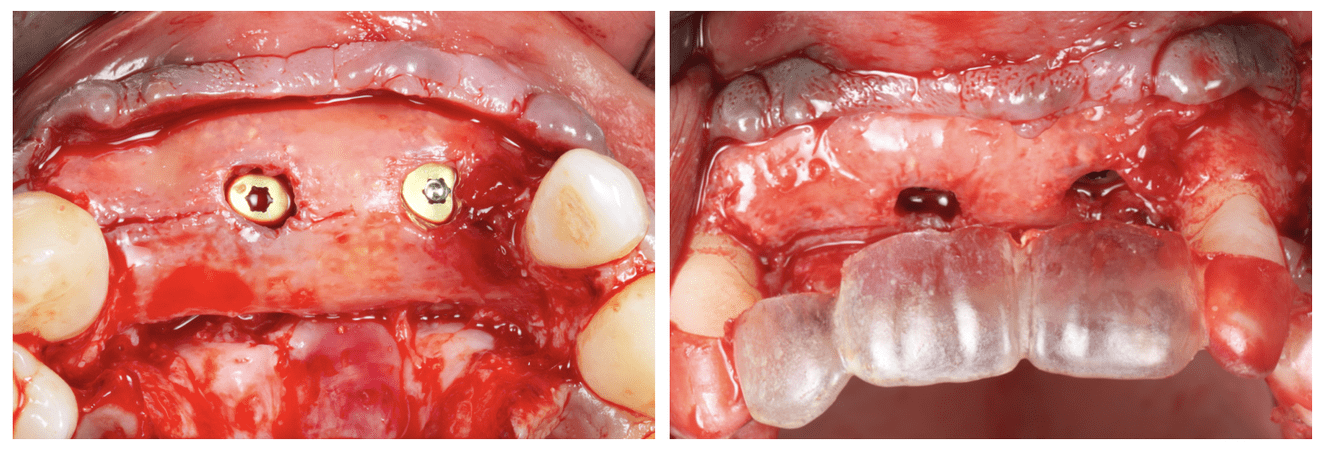
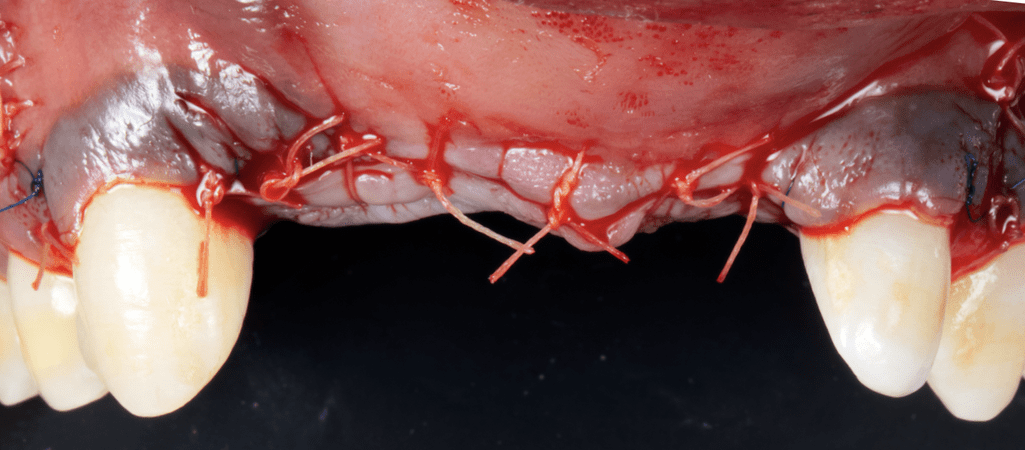
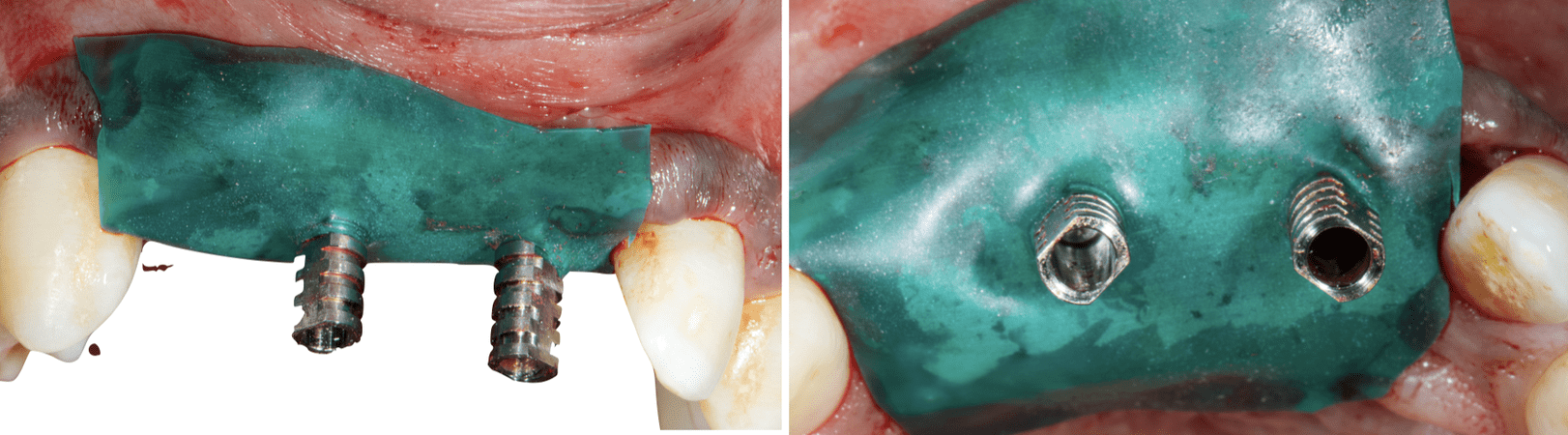
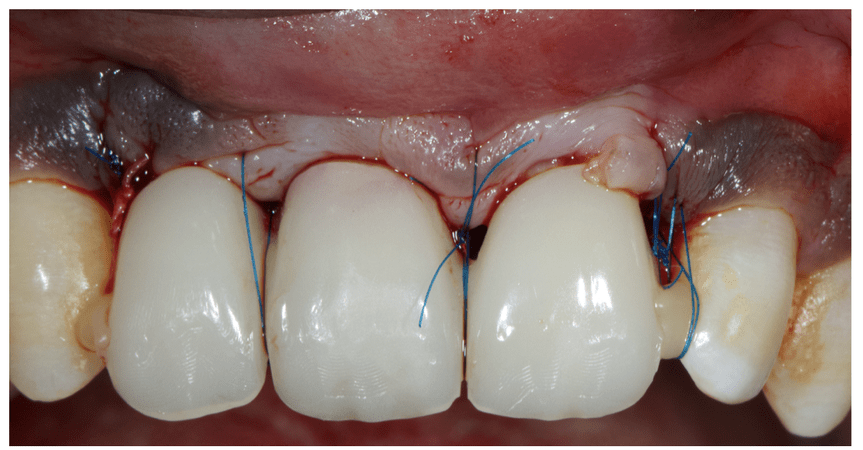
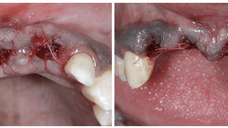
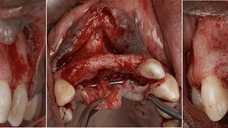
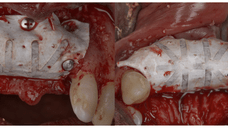
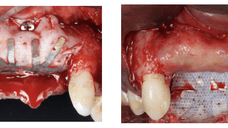
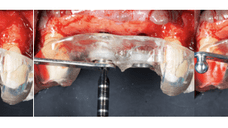
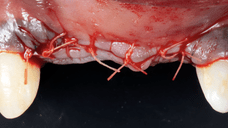
To address the horizontal deficiency, a guided bone regeneration (GBR) procedure was scheduled. The bone graft consisted of a hybrid mixture of xenogenic and allogenic biomaterials, selected for their osteoconductive and volume-stable properties. These were covered with a titanium-reinforced non-resorbable PTFE membrane to provide space maintenance and mechanical stability during the regeneration phase.
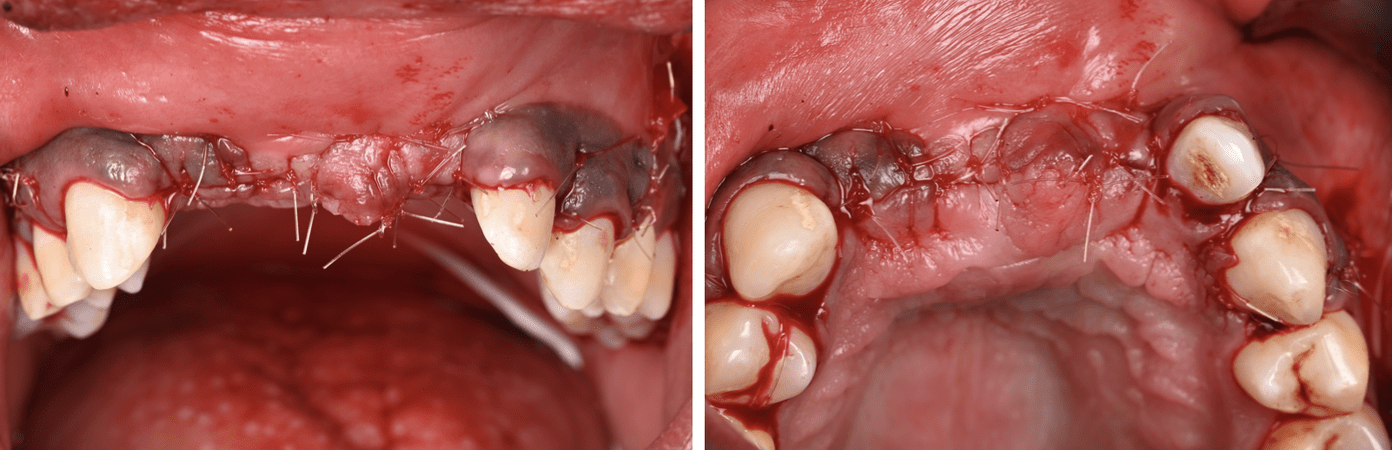
The surgical site was carefully closed to ensure primary tension-free closure, and the patient was placed on an appropriate postoperative protocol. Healing was uneventful, and the membrane was removed after the standard healing period. A nine-month interval was allowed for full integration and maturation of the graft before reevaluation.
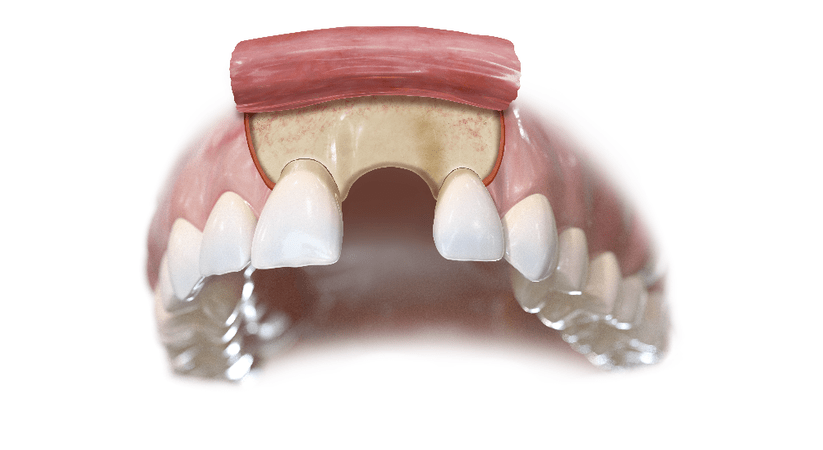
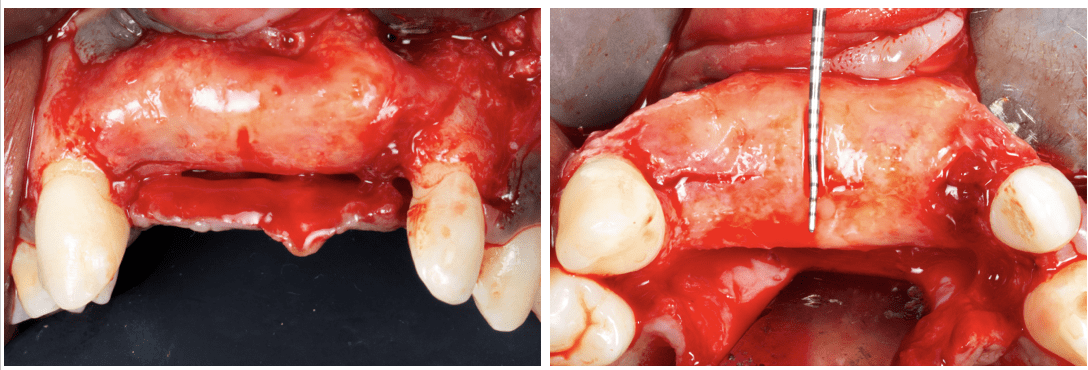
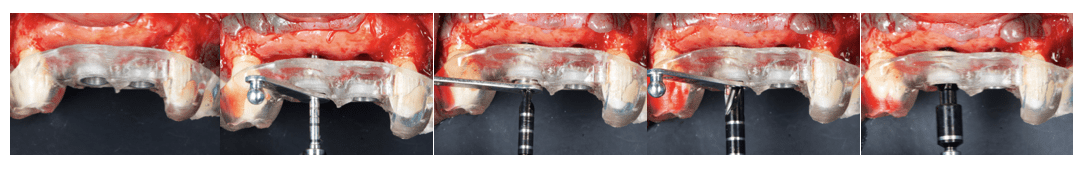
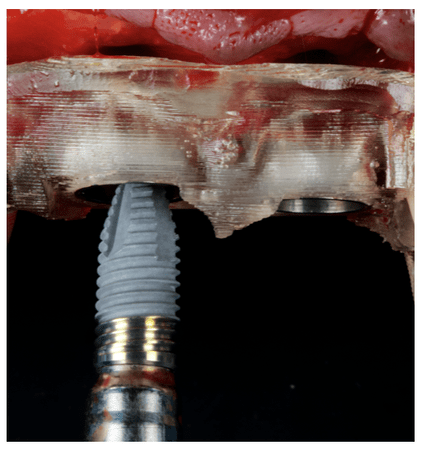
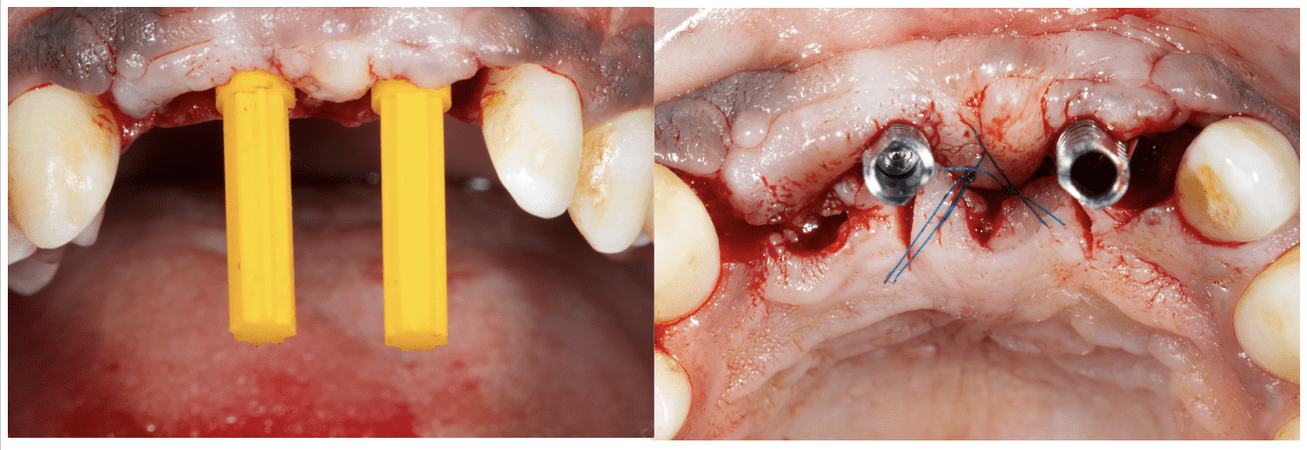
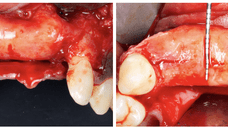
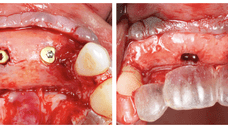
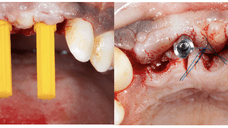
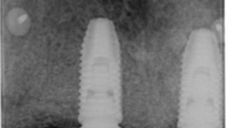
A second CBCT was performed and digitally merged with an intraoral STL file of the maxillary arch. This allowed for a precise three-dimensional assessment of the regenerated bone and facilitated virtual implant planning using DTX Studio software. According to the original aesthetic project, implants were planned in positions 11 and 21, with a cantilever extension replacing tooth 12.
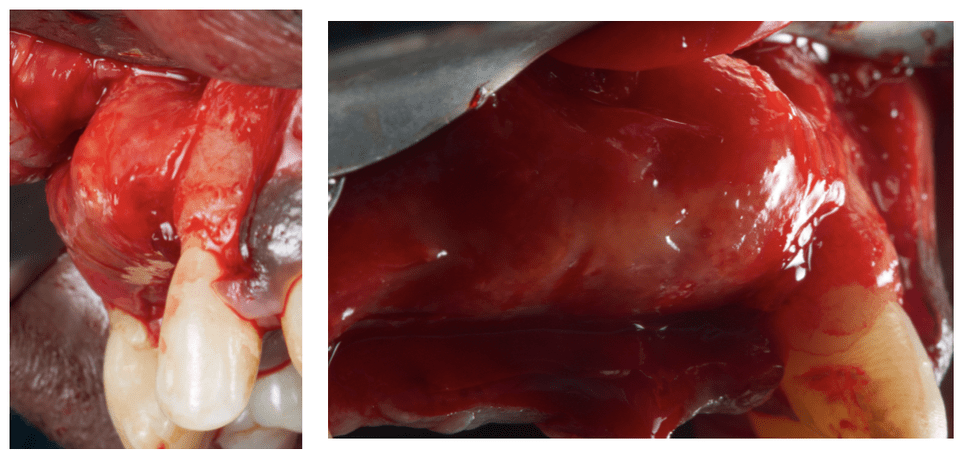
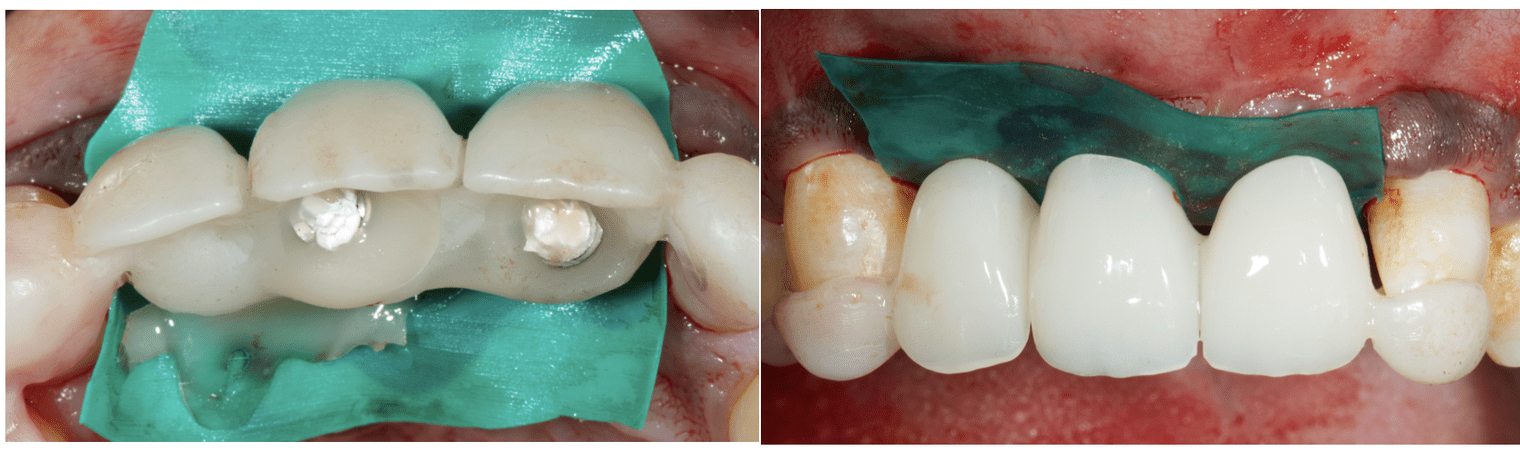
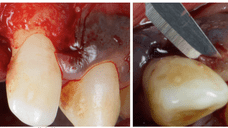
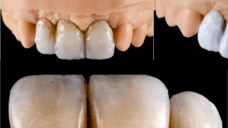
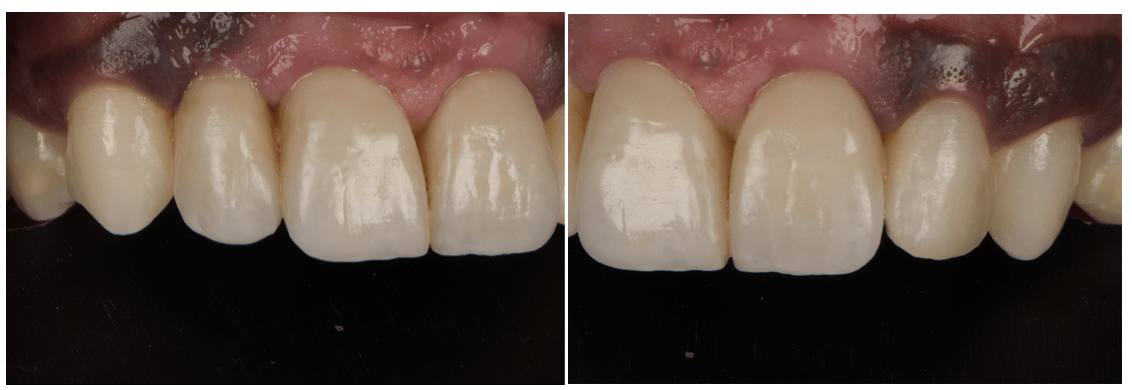
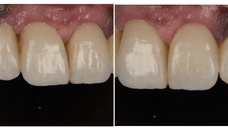
Implant placement was fully guided using a stereolithographic surgical guide to ensure accuracy and parallelism. Following successful osseointegration, a screw-retained provisional bridge was fabricated and inserted to condition the soft tissues and shape the emergence profile. The final emergence contours were carefully captured using a digital impression and transferred to the dental technician for final prosthesis fabrication.
Follow-up & Outcome
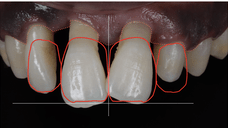
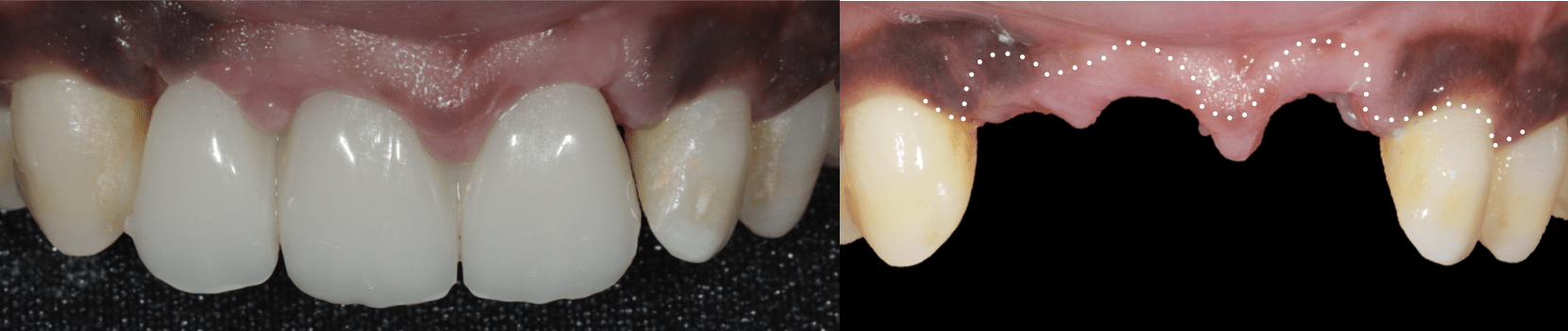
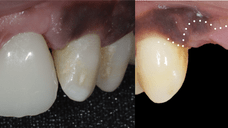
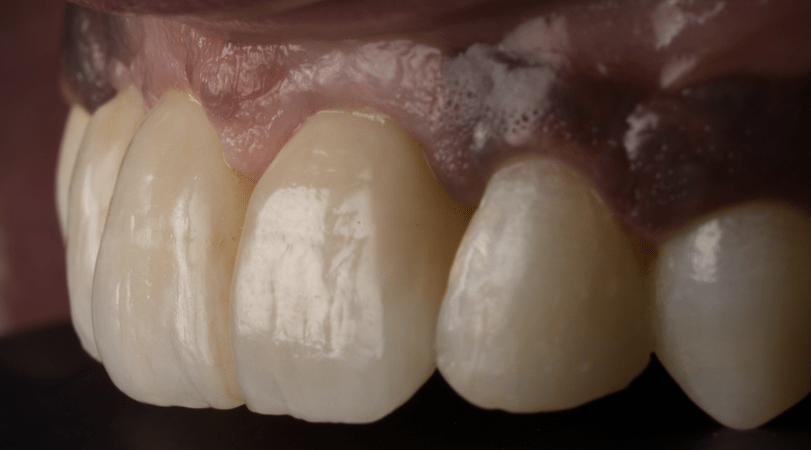
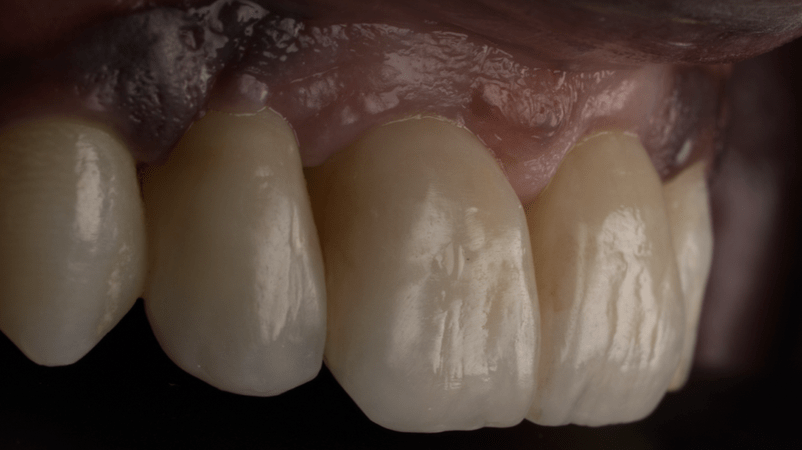
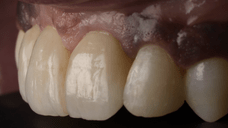
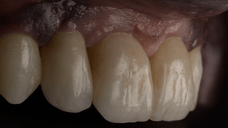
The definitive prosthesis was designed based on the emergence profile established by the provisional. The bridge was milled in high-translucency zirconia and selectively stratified with ceramic to enhance optical properties and achieve a natural esthetic result. It was torqued onto multi-unit abutments at 15 N.cm to ensure stability and retrievability.
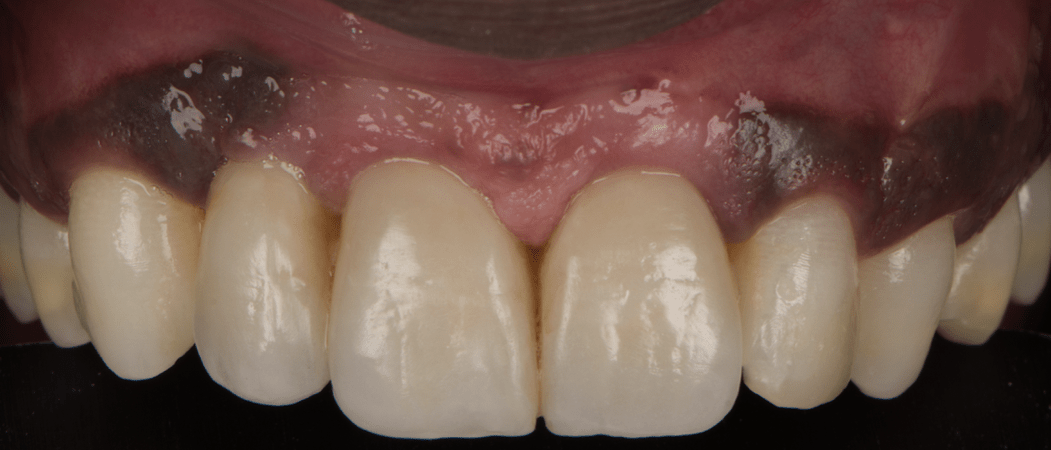
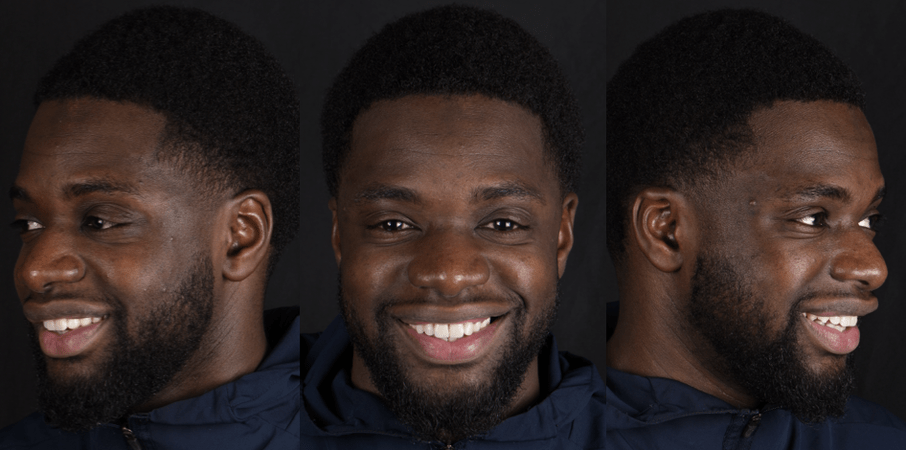
The soft tissue architecture around the implant-supported bridge exhibited harmonious integration, with well-defined interdental papillae and a natural-looking gingival margin. The prosthesis blended seamlessly with the surrounding dentition, respecting the initial virtual aesthetic plan approved by the patient.
The patient expressed high satisfaction with both the functional and aesthetic outcomes. Speech, phonetics, and comfort were evaluated during follow-up visits, and no complications such as mucositis, peri-implantitis, or mechanical issues were reported. Radiographic monitoring confirmed stable crestal bone levels around the implants.
The patient has been enrolled in a structured maintenance protocol, including clinical and radiographic evaluation every six months. At each recall, the prosthesis is inspected, hygiene is reinforced, and any necessary adjustments are made. The long-term prognosis is favorable due to careful planning, surgical precision, and continuous follow-up.
Team Members / Acknowledgements
Luis Saraiva (Dental Technician), Dr. Marwan Daas, Dr. Benjamin Attuil, Dr. Rony Cohen-Hadria (treatment planning and case elaboration)