Immediate implant and immediate loading in the aesthetic zone
A 72-year-old female patient was referred with a chief complaint, “I want to restore my central incisor". She refers no relevant medical history. Her past dental history included extensive restorative treatment with metal-ceramic crowns in the maxillary and mandibular arches.
A facial and dental analysis was performed using extraoral and intraoral pictures, CBCT, and conventional impressions to aid in developing a complete diagnosis and treatment plan.
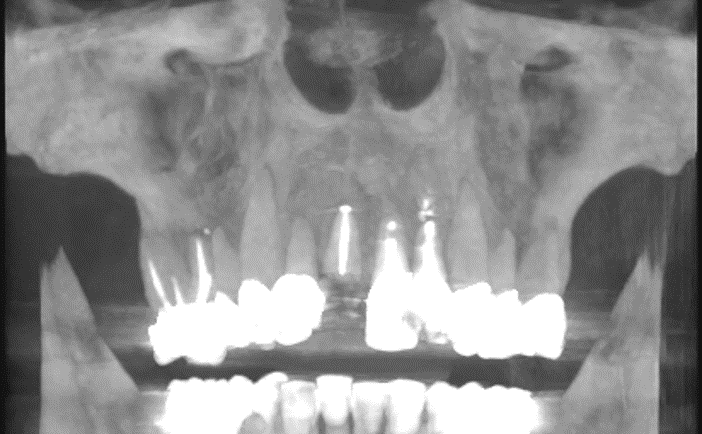
In the intraoral analysis, the patient presented with decayed teeth #12, #11, #21, #22 FDI (#7, #8, #9, #10 US), crown fracture #11 FDI (#8 US), and over-contoured maxillary crowns on the central and lateral incisors.
A challenge with this treatment was that the patient refused a removable partial denture as a provisional prosthesis. As a result, it was necessary to place an immediate fixed partial prosthesis and achieve high primary stability on the implants as well as meet the patient expectations for high aesthetics.
The patient visited the surgical dental practice as an emergency due to a fracture of tooth 11. Her wish included not only a new restoration of the fractured tooth, but also a more aesthetic new restoration of the entire anterior teeth of the upper jaw. The patient was informed in detail about the course of treatment, risks, prognosis, costs and treatment alternatives. In terms of general medical history, there were no other special health features.
The decision for immediate implant placement was based on several reasons: This procedure saves the patient and the dentist time and effort, reduces costs and patient morbidity, and minimizes changes in the bone and soft tissue. The positions of implants 12 and 22 were determined using the extraction sockets as a reference. An anterior fixed partial denture with two pontics was planned on the implants, which could also optimally use for soft tissue conditioning. The patient discussed the desired tooth color together with our dental technician, who also included the patient's aesthetic wishes in the design. The treatment was planned in advance according to the patient's wishes, and the implant positions were determined using NobelClinician planning software.
Evaluation & Diagnosis
Progress & Completion
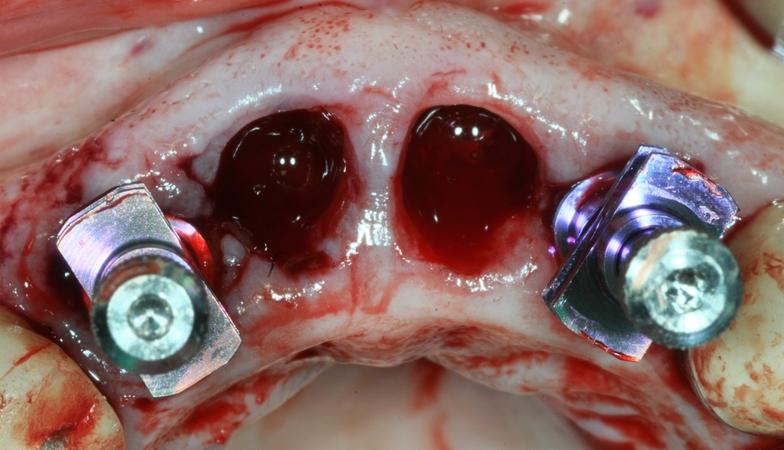
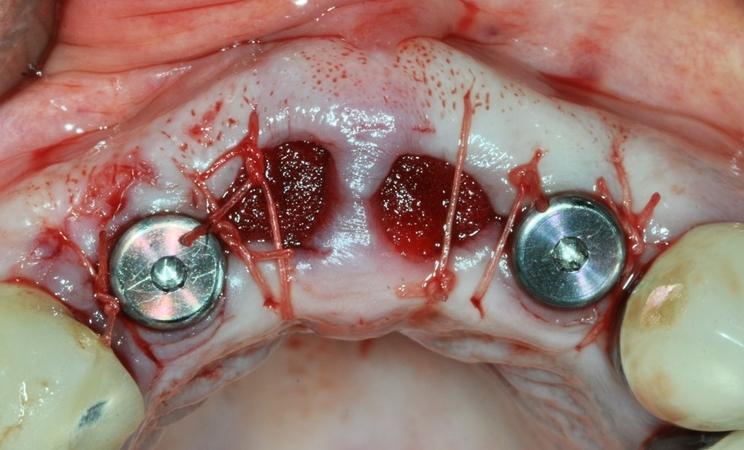
The procedure was performed freehand to be able to react to any surprises after the extraction. The existing bone quality was assessed as good, which allowed us to perform immediate implant placement in the maxilla. The careful extraction of teeth 12 to 22 was carried out properly and without further complications. A flapless approach was chosen to avoid stressing the hard and soft tissues as much as possible. This procedure ensures us a better aesthetic design of the tissue structures. The extraction sockets in region 11 and 21 were thoroughly cleaned, filled with collagen cones and closed with adaptation sutures. After appropriate pretreatment, a NobelActive TiUltra NP implant with a diameter of 3.5 mm and a length of 15 mm was placed in each of the alveoli of teeth 12 and 22 according to the prescribed drilling protocol. The root-expanding implant body provides continuous bone compaction, while the dual-bladed tip allows minimal osteotomy. These features support the achievement of high primary stability. The narrow tapered coronal area and integrated platform switching maximize alveolar bone volume and soft tissue support. Furthermore, the sharp implant tip grants the possibility to adjust the implant alignment for optimal prosthetic restoration and esthetic results. The situation was then imprinted with attached laboratory analogues so that we could immediately fabricate and place a customized provisional.
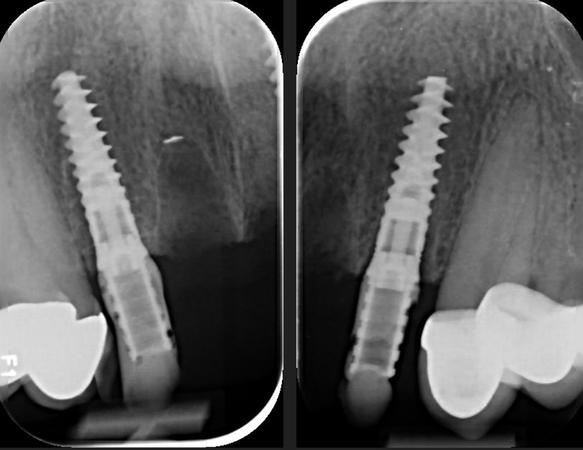
The peri-implant healing process also depends on the microtopography of the implant surface. Basically, titanium implant surfaces are processed using different methods. Among others, the oxidized TiUnite surface has proven itself. The thickened, moderately rough titanium oxide layer with high crystallinity and a high phosphorus content has been shown to promote osseointegration. The NobelActive implant system, with its modified design, is considered a pioneer in this field, has been on the market for ten years and has been scientifically tested in about 42 clinical studies (more than 14,300 original implants in about 2,600 patients). Finally, the two implants were checked for their exact fit with the help of inserted laboratory analogues using X-ray images.
Insertion of the provisional restoration
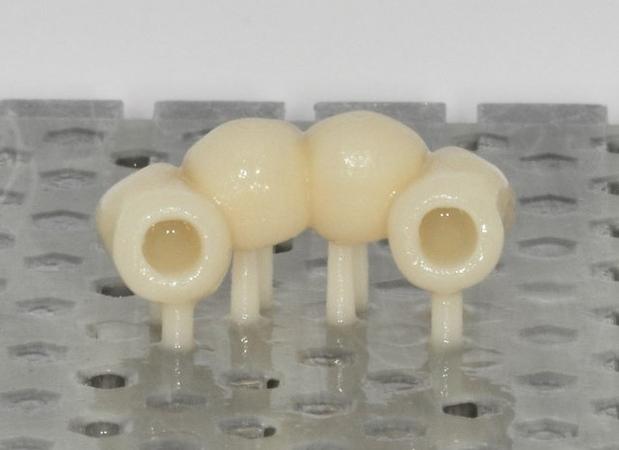
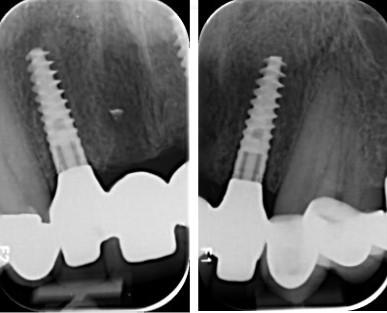
Depending on the previously determined tooth shade, a provisional aesthetic fixed partial denture made of Vita Flow resin teeth was fabricated in the dental laboratory and placed on the implants. Since we could not be sure before implant placement that we would achieve the necessary primary stability for immediate loading of the temporary restoration, the laboratory first made us a removable provisional prosthesis that served as a placeholder after the operation. Since the implant placement took place as planned and we achieved the stability of more than 35 Ncm required for immediate loading, we were able to make another impression of the situation with screwed-in impression posts so that the laboratory directly fabricated the fixed provisional restoration for us. Fitted with the removable provisional, the patient waited for the fixed version in our practice. An easy way to build up an implant is to use the Nobel Biocare NP abutment (temporary abutment element). To create a natural shape of the gingival line and to shape the soft tissue around the implant for an authentic appearance, an artificial gingival cover was used on a model. The shape of this provisional fixed partial denture was slightly over-contoured in the cervical area to apply gentle pressure on the soft tissue. The purpose of this procedure was to ensure that the form of the peri-implant mucosa in the area of the implant was optimally shaped. If necessary, this process can be repeated during the healing phase by adding composite resin material to apply targeted pressure. Finally, the correct fit was checked with the help of a radiograph and the patient was discharged from the practice for the duration of the soft tissue shaping, in this case for about four months.
Transfer of the soft tissue structure
The soft tissue structure shaped during the therapeutic period formed the basis for the customized abutments and the final restoration. First, it was necessary to transfer the shaped appearance of the soft tissue line to the model of the implant by fabricating customized impression posts. For this purpose, the provisional fixed partial denture was removed. The provisional prosthesis was then screwed onto the laboratory analogue NP outside the mouth and covered with a kneadable silicone material. After the silicone had hardened, the prosthesis was removed from the lab analogue and the impression posts were attached to the lab analogue embedded in the silicone. The space between the impression posts and the silicone was filled with composite resin material. These impression posts were then used to make the impression of the implants with a previously fabricated custom impression tray. The master cast now exactly matched the shape of the soft tissue profile in the area of teeth 11 and 21. While the patient was again satisfied with the long-term provisional, the dental technician fabricated the definitive crown.
Placement of the definitive crown
After completion of the definitive treatment, the patient came back to our practice. After removing the therapeutic provisional, the peri-implant soft tissue was healthy as expected, well supplied with blood and shaped as desired in region 11 and 21, so that we were able to place the definitive restoration made of zirconium oxide without any complications. The prosthetic restoration blended into its natural environment completely invisibly and the patient regained her radiant smile. It is the comparison between the initial situation and the final restoration that confirms our approach. The radiological comparison between the initial situation and the completed work also revealed a good fit of the prosthesis and an absolutely satisfactory result.
Follow-up & Outcome
In the meantime, the patient had additional treatments performed in the maxillary posterior region. The bone level between the placement of the definitive restoration and the follow-up appointment was monitored, but there was no sign of tissue recession. To date, the treatment continues to sit stably, the peri-implant bone line remains where we wanted it to be, and there is little discernible difference from the natural adjacent teeth.
This treatment description shows that immediate implant placement in the anterior region is an effective treatment method when indicated and with the correct technique. Precise diagnosis, individual consideration of the patient's wishes and careful treatment planning are decisive for the success of such procedures. Comprehensive aftercare and consideration of aesthetic aspects also contribute to a successful treatment outcome.
Questions
Ask a questionDid you fill the gap with xenograft between implants and labial bone in extraction sockets?
In the area of pontics socket preservation? Nice soft tissue biotype, no need for connective tissue graft? When did you final prosthetic structure. Thanks.
In the area of pontics socket preservation? Nice soft tissue biotype, no need for connective tissue graft? When did you final prosthetic structure. Thanks.
Did you fill the gap with xenograft between implants:
No, only an adaptation through individual button sutures and protection of the gap between the implant and bone by the provisional
4 month after surgery we finalised the prosthetic
Hello and thanks for this beautiful case. I want to know after the immediate implant placement, what did the patient have
Team members








































Do you have to do crowns on upper canines and posterior teeth for better color and shape ?
or did you match color with only canines ?
Very good job!
or did you match color with only canines ?
Very good job!
In reply to Do you have to do crowns on upper canines and posterior teeth for better color and shape ? by Anonymous
Yes we did ,in a second phase , new crowns on the upper canines!
best regards