Mucosa Management using the Buccal Pedicle Flap technique
Video highlights
- Mucosa management around implants
- The buccal pedicle flap technique
Dr. Giorgio Tabanella continues his lecture with a focus on the mucosa management and what can be done to really improve the quality of the mucosa to prevent implant and biological complications.
He recaps that we need to have a 2 mm band of keratinized mucosa. There also needs to be a good quality of the buccal bone balcony with more than 1.4mm of bone thickness around the implant neck. According to literature, about one-third of implants may need a connective tissue graft. This kind of procedure is the gold standard. Patients in need for this kind of procedures mostly experienced failures or complications or have received multiple implants. With these patients, common sense and a simplified procedure is required. Dr. Tabanella uses the buccal pedicle flap technique every time he needs to manage the soft tissue and needs to boost and improve the peri-implant mucosa.
He starts to explain the procedure with a patient case. A young female patient, who lost an upper canine due to a traumatic extraction, came to the office. An alternative treatment with the eruption of the canine was not possible, so the canine needed to be extracted. The clinician who treated the patient previously, extracted the tooth and placed an implant, which failed. A third surgical procedure including implant placement and guided bone regeneration was performed and failed. So, when the patient entered Dr. Tabanella’ s office, she was already a difficult patient because of all the failures. When looking at the case, there are already some limitations in terms of the biology. At first glance, there is a poor quality of the mucosa, with the keratinized tissue being split in two different parts. There is no convexity present, and a recession on the lateral and on the premolar. The palatine rugae are visible through the buccal aspect of the site. He explains that he approached the case by thinking how he could improve the quality of the peri-implant mucosa. As the palatine rugae are visible, there is also a need to restore the pink aesthetics as the vertical dimension is missing, next to some vertical collapse of the tissue, a class II mobility is present, and the lateral incisor needs to be taken care of. As part of the treatment, the clinician should visualize the final result, so there is a clear understanding of how the implant is going to be placed. This helps in deciding which kind of bone and tissue augmentation is required. A digital wax-up helps Dr. Tabanella to identify that he has a chance to get a pseudo-papilla on the distal aspect of the canine, but it will be very complicated to obtain the pink aesthetics on the mesial aspect of the canine, as there is recession present on the neighboring dentition. Additionally, he must deal with attachment loss on the lateral incisor, as he can see on his digital planning software. When talking to the patient and explaining the treatment, he needs to mention that there might be chance of pink porcelain to restore the amount of pink tissue missing on the mesial aspect. If something goes wrong, the situation will be worse than when the patient first came in. He shares that the treatment plan will foresee a guided bone regeneration, followed by a healing period to let the bone mature, an implant placement and the extraction of the lateral incisor due to a 9mm bone loss. This tooth will also be replaced by an implant, and the case will be finalized with an implant in the lateral and canine region at the same time. On the images, the remnants of the previous bone graft are visible, and the anatomy is unusual due to the buccal collapse of the ridge after the tooth extraction. It is not common to see a buccal plate with this minimum amount of vertical bone and the complete absence of the palatal wall. As Dr. Tabanella highlights, all of this is already known before the flap is opened, due to digital technology. The navigation needs to happen inside of the patient’s tissue, so the digital wax-up, has all the parameters such as the insertion depth of the implant which is crucial for the perfect emergence profile and important for the maintenance of the implant. The buccal plate being very thin is not a surprise, so he knows that he will not be able to place any screws and pins. The recession means that the periodontal ligament has been lost on the neighboring dentition which results in a missing blood flow in the region. The bone regeneration procedures should be kept simple and predictable, according to Dr. Tabanella. He emphasizes he cannot go beyond the bony peaks, if he wants to be on the safe side, due to the blood supply coming from this area. The guided bone regeneration is done with a mixture of autologous and demineralized bovine bone as well as an absorbable membrane. In this specific situation a block graft can not be stabilized and therefore is not an alternative for the regeneration. The stabilization of a titanium mesh will be difficult and complicated, so the best option is the use of a resorbable membrane. After 7 months of healing Dr. Tabanella is ready to place an implant and load the implant another 4 months later, simultaneously he plans to extract the lateral incisor. He did not extract the incisor as the bone regeneration was able to repair the palatal wall of the lateral incisor. He performed a buccal pedicle flap at this point. Dr. Tabanella continues to explain, that a buccal pedicle flap allows him to obtain a slope of 10 degrees, which the soft tissue can tolerate well. Pseudo-pocketing is not observed in this kind of situation, which is known from periodontal osseous surgery. He points out that every time a need to change the architecture on the bone level needs to be changed and a slope of 10 degrees is maintained, there will be no rebound effect of the pocketing. This result can be transferred to implant dentistry. According to Dr. Tabanella, the buccal pedicle flap is a simple procedure as it is a pedicle not a rolled flap. A substantial amount of soft tissue gain can be achieved in terms of soft tissue volume. He demonstrates this with one of the cases, that have been published. This procedure can be performed in anterior and posterior regions. In addition, a good depth of the vestibulum can be obtained, which is usually lost after guided bone regeneration. This simple procedure brings the same result without the need for invasive and painful interventions.
Dr. Tabanella takes us through step-by-step through the procedure: he starts from the palatal aspect with a horizontal incision from the occlusal, moving on to the buccal aspect. A partial thickness flap is done, and the edge of the flap is fixated using a concave healing abutment. On the buccal, two vertical releasing incisions are made and a cut-back to get what Dr. Tabanella calls “wrinkles” or “waves” within the tissue. The purpose of the buccal pedicle flap and the rational behind is to get space on the buccal aspect. Granulation tissue will form in that space and will help the boosting of the peri-implant mucosa. He emphasizes that this a flap not a free graft, so there is little risk of failures. He continues to show the procedure from the buccal aspect: two vertical incisions and the cut-back because the flap must be really released. Even though it does not look great in the first days, mother nature will create a perfect bridge with a soft tissue which can also be observed with block grafts. When a block graft or guided bone regeneration is performed, a bridge between the augmented and native bone can be observed. He explains again that a partial thickness flap is created in which he needs to pass the muco-gingival junction. By bringing keratinized tissue from the palatal aspect to the buccal aspect a significant amount of keratinized mucosa around the neck of the implant can be created. For the mandible, at least 2mm in the lingual aspect need to remain which is the limitation for the lower arch. Just with the placement of the abutment a certain flexibility remains, and the flap is stabilized by 5 or 6 monofilament sutures on the buccal aspect. Looking from the sagittal point of view, the space on the buccal aspect is visible. A modified version of this procedure is the use of creosTM mucogain or any collagen matrix. The result is achieved by the flap design. Coming back to the patient case, Dr. Tabanella explains that he performed the buccal pedicle flap at the time of uncovery. He left the embrasure open on purpose. He is also aware of the amount of creeping attachment that he can get with the buccal pedicle flap, which about a maximum of 2.5 mm, with an average of 1.5mm. On the x-rays taken 1.5 years post-op, real newly formed tissue is present. There is a junction line between the native and the creeping mucosa around the neck of the implant. It can be removed, in case of any aesthetic issues, with a diamond bur. With a little bit more patients, this line will disappear. In the presented case it took around two years to disappear. Dr. Tabanella shares that he applied periodontal principles to the implant dentistry. He created a slope of 10 degrees, brought tissue from the buccal aspect, and sculptured the emergence profile with a concave titanium or zirconia abutment. Important is that the porcelain is stratified within the connected tissue or junction epithelium, as that compartment will be in contact only with the titanium or zirconia abutment. Comparing the results post-op to before and at the delivery of the final restoration, after 1.5 years creeping attachment is present, after 3 years a better stabilization can be seen and after 4 years it has even grown a little bit more. The tissue looks better year after year. The result looks like the result of a connective tissue graft without performing a grafting. After 8 years, a keratinized tissue band of 7-8mms has formed around the neck of the implant with a good convexity of the pink tissue, following the convexity of the final restoration.
Dr. Tabanella continues to validate the result by using a probe around the neck of the implant – which is something he rarely does as he doesn’t want to disrupt the fragile adhesion between the connective tissue, the junction epithelium, and the abutment. When he uses his probe after 8 years to evaluate the presence of pseudo-pocketing, he finds 3 mm of sulcus and bleeding due to forcing the probe into the connective tissue. Summarizing the main points of the buccal pedicle flap: minimally invasive, can be performed in anterior and posterior regions, for single and multiple units and predictability. Obtaining a restitution integrum of the depth of the vestibulum is so crucial to avoid food impaction after guided bone regeneration and also helps to reduce the risk of major and invasive types of surgical procedures. The increase of thickness is three-dimensionally with an increased band of keratinized tissue as well. What about long-term follow up? Dr. Tabanella shares a study which compared patients receiving the buccal pedicle flap and second stage surgery versus patients receiving a connected tissue graft versus patients receiving a traditional crestal incision at the time of uncovery. In average a natural boosting after the delivery of the final restoration of 1.5 mm with the buccal pedicle flap versus 0.33 with the connected tissue graft or 0.51mm with the crestal incision could be observed. When looking at the thickness height of the soft tissue and keratinized tissue, the buccal pedicle flap was able to perform better than all the other types of technique that were utilized in the study.
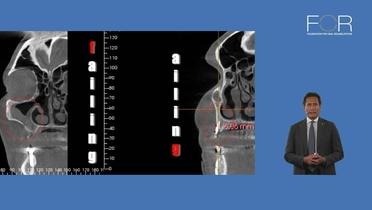
But what about ailing and failing dental implants? asks Dr. Tabanella. He shares a case which has “a little bit of everything”: a 40-year-old female patient came in, with the fever, pus and suppuration coming from the right nostril. There was an oro-antral communication and of course, pain. Looking at the peri-apical radiographs, an implant is placed on the distal aspect, an implant also placed on the mesial aspect and, again, an implant is connected to a natural tooth. The implant on the mesial aspect has exposed threads, the tooth shows endodontic fillers, periapical chronic lesions, and decay. Exploring the looking the distal bridge with the two implant connected, we see that the mesial implant is completely disconnected, so it's a failing dental implant. This case presents sinus grafting failures, endodontic failures, prosthetic failures, peri-implant bone loss, which is not peri-implantitis, and finally, peri-implantitis. The mesial implant is an ailing dental implant, the middle implant, is a failing dental implant. Due to bacterial contamination of the graft, the patient shows pus. The CBCT shows that the right maxillary sinus is full of pus without drainage, causing the patient a lot of pain. Moving on to the clinical aspects of the case, there is a mobile implant, this implant is exfoliating and that is why this patient is also showing sinusitis with suppuration. The implant can be very easily removed, using just a hemostat. A thorough degranulation of the sinus took time. The incision starts at the tooth which is failing due to endodontic failures. It takes a lot of time as well to remove the granulation tissue, entering the sinus through the oro-antral communication and then stabilizing the sinus membrane elevation with multiple spongeous collagen. Closing the oro-antral communication is a prerequisite for bone augmentation later. When explaining his treatment plan for the patient, he says that he is going to use the distal implant, which is healthy, and the mesial implant which is an ailing dental implant, as a strategically convenient type of implant. The mesial implant will support a reinforced provisional which the patient will receive during the long treatment time. The first surgical phase is closed by inserting a lot of spongeous collagen inside the sinus. Next, he shows images after implant removal and 6 months after the surgery. When looking at the peri-apical x-rays, one can see a change in the bone architecture. What has changed is the amount of bone that could be gained just by shifting the sinus membrane more apically and inserting spongeous collagen and closing, of course, the oro-antral communication. A CBCT confirms that the sinus is completely empty and clear of inflammation. The sagittal view shows the amount of bone through the surgical intervention that focused on the closing of the oro-antral communication. The reinforced provisional already helped to sculpture the soft tissue and the next step is the implant placement. He enters the sinus again with a vertical approach, also applying a minimal invasive approach as only 4mm of residual bone in the area of the implant placement. Applying spongeous collagen will help to protect the Schneiderian membrane followed by demineralized bovine bone, placed with osteotomes. The membrane is shifted very carefully by slowly placing the bone particles. The sinus elevation is extended slighty to the area of the middle implant. The most anterior implant is an ailing dental implant with exposed threads and placed slightly buccally. This type of implant will not allow for a nice pink aesthetic, so the implant is removed and the residual statomocytes are treated as an immediate placement site. After removing the implant, the socket is cleaned from granulation tissue and prepared with a twist drill to receive a new implant. Dr. Tabanella is performing a guided bone generation to obtain what is defined as the buccal bone balcony, a good thickness of vital bone around the neck of the implant. Literature mentions at least 1.4-1.5 mm of vital bone around the neck of the implant to ensure for long-term stability. As a study showed, implants which had less than 1.4 mm vital bone were likely to show advanced peri-implant bone remodeling. He is inserting the implant and tries to expand the buccal plate with the osteotomes, followed by a guided bone regeneration with the idea of getting the buccal bone balcony. He explains that the idea, and part of the treatment planning was also to perform simultaneously immediate loading. With just two surgical phases, he is trying to solve a situation which was difficult to begin with, just one surgical phase to reduce the oro-antral communication and to get also bone inside the sinus. As the implant is sufficiently stable, he will immediately load the implant. He uses the immediate abutments as a pivot to stabilize the resorbable creosTM collagen membrane. The membrane is additionally fixated with pins to stabilize the bone particles. After some time a new provisional is created to sculpture the pink aesthetic result a bit better – using the pressure on the tissue by the provisional – without performing a soft tissue manipulation. Of course 100% of the bone was augmented in these sides, Dr. Tabanella points out. After the immediate loading of the implants, a second set of provisionals was inserted. The design helped to sculpture the concave profile on the buccal aspect and on the lingual aspect a slope was created to support the cleansing properties and guide the slope from palatal to buccal. He concludes the case by showing the follow-ups from 4 and 6 years. Summarizing the lecture, Dr. Tabanella emphasizes that failures can be turned into a successful result.
References
[1] Vela X, Méndez V, Rodríguez X, Segalà M, Gil JA. Soft tissue remodeling technique as a non-invasive alternative to second implant surgery. Eur J Esthet Dent. 2012 Spring;7(1):36-47. PMID: 22319763.
[2] Cosyn J, De Bruyn H, Cleymaet R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: a 1-year prospective study. Clin Implant Dent Relat Res. 2013 Dec;15(6):847-57. doi: 10.1111/j.1708-8208.2012.00448.x. Epub 2012 Feb 29. PMID: 22376232.
[3] Tabanella G. The buccal pedicle flap technique for periimplant soft tissue boosting. Int J Esthet Dent. 2019;14(1):18. PMID: 30714051.
[4] Brägger U, Lauchenauer D, Lang NP. Surgical lengthening of the clinical crown. J Clin Periodontol. 1992 Jan;19(1):58-63. doi: 10.1111/j.1600-051x.1992.tb01150.x. PMID: 1732311.
[5] Harris RJ. Creeping attachment associated with the connective tissue with partial-thickness double pedicle graft. J Periodontol. 1997 Sep;68(9):890-9. doi: 10.1902/jop.1997.68.9.890. PMID: 9379335.
[6] Bömicke W, Gabbert O, Koob A, Krisam J, Rammelsberg P. Comparison of immediately loaded flapless-placed one-piece implants and flapped-placed conventionally loaded two-piece implants, both fitted with all-ceramic single crowns, in the posterior mandible: 3-year results from a randomised controlled pilot trial. Eur J Oral Implantol. 2017;10(2):179-195. PMID: 28555208.
[7] Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Analysis of risk factors for cluster behavior of dental implant failures. Clin Implant Dent Relat Res. 2017 Aug;19(4):632-642. doi: 10.1111/cid.12485. Epub 2017 Mar 22. PMID: 28332286.
[8] Tabanella G, Nowzari H, Slots J. Clinical and microbiological determinants of ailing dental implants. Clin Implant Dent Relat Res. 2009 Mar;11(1):24-36. doi: 10.1111/j.1708-8208.2008.00088.x. Epub 2008 Apr 1. PMID: 18384407.
[9] Giorgio Tabanella and Peter Schupbach. “A Peri-Implant Soft Tissue Biopsy Technique to Analyze the Peri-Implant Tissue Sealing: A Non Invasive Approach for Human Histologies”. EC Dental Science 16.2 (2017): 93-99.
[10] Urban IA, Nagursky H, Church C, Lozada JL. Incidence, diagnosis, and treatment of sinus graft infection after sinus floor elevation: a clinical study. Int J Oral Maxillofac Implants. 2012 Mar-Apr;27(2):449-57. PMID: 22442787.
[11] Vela X, Méndez V, Rodríguez X, Segalá M, Tarnow DP. Crestal bone changes on platform-switched implants and adjacent teeth when the tooth-implant distance is less than 1.5 mm. Int J Periodontics Restorative Dent. 2012 Apr;32(2):149-55. PMID: 22292143.
[12] Zuffetti F, Capelli M, Galli F, Del Fabbro M, Testori T. Post-extraction implant placement into infected versus non-infected sites: A multicenter retrospective clinical study. Clin Implant Dent Relat Res. 2017 Oct;19(5):833-840. doi: 10.1111/cid.12523. Epub 2017 Jul 26. PMID: 28744958.