Vertical ridge augmentation in posterior mandible
Bone augmentation procedures are routinely applied in cases of alveolar ridges deficiency in order to achieve optimal bone support for osseointegrated dental implants, and ensure successful and long terms outcomes in dental implant therapy. GBR was initially used to treat simple defects, including dehiscence and fenestration defects. The application of GBR for horizontal and vertical ridge augmentations is well documented with high implant survival rates and low complication rates.
Long term results concluded that vertically augmented bone using GBR techniques responds to implant placement in a similar fashion to native bone.
The results of clinical and histologic studies of ridge augmentation with GBR indicated that anorganic bovine bone-derived mineral (ABBM) mixed with autogenous particulate bone may be suitable material for staged localized ridge augmentation in both horizontal and vertical dimensions. This clinical report describes and demonstrates the successful use of autogenous particulate bone, anorganic bone mineral and barrier membranes to reconstruct severe alveolar bone defect.
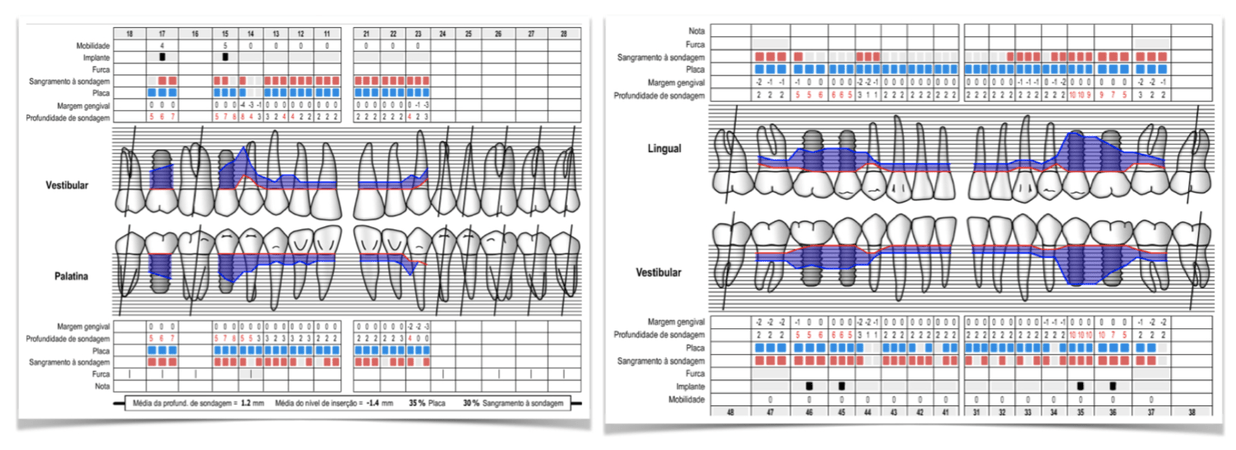
Evaluation & Diagnosis
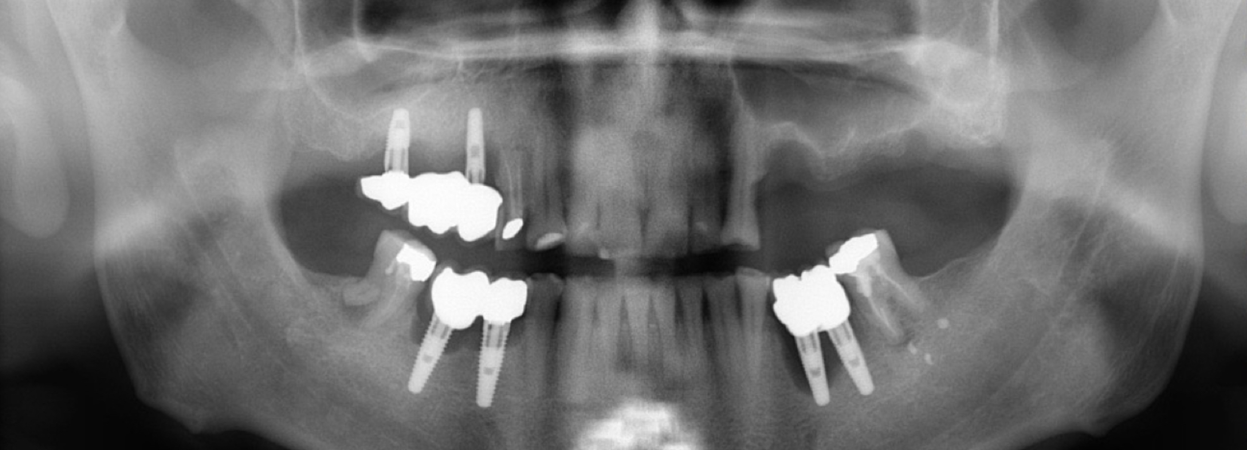
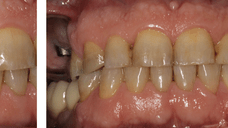
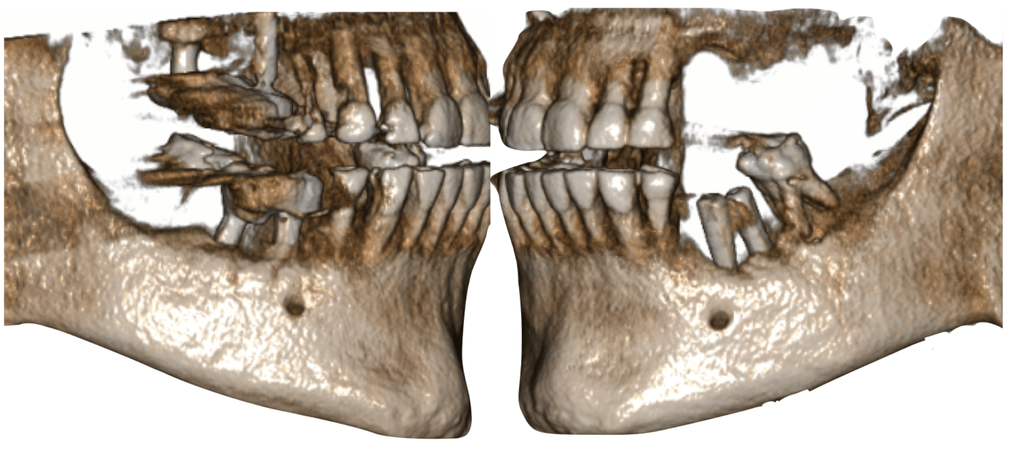
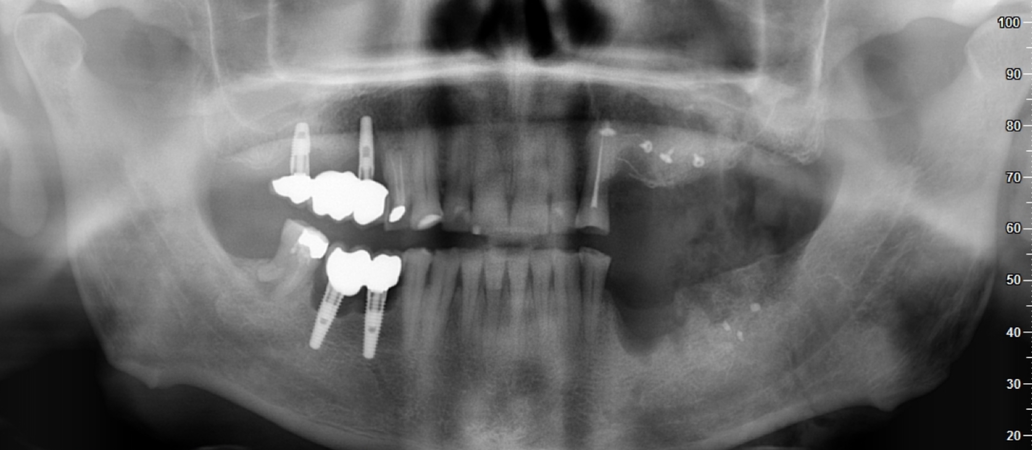
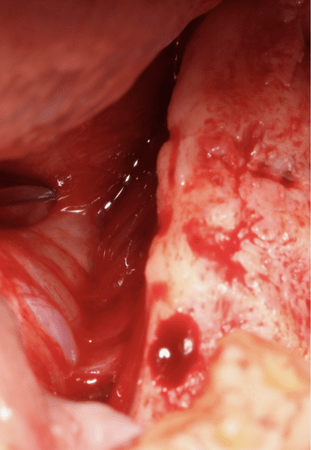
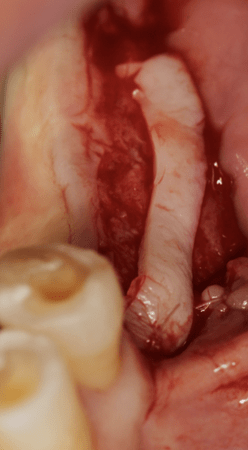
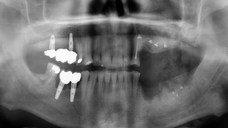
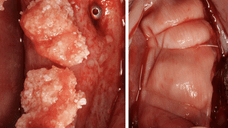
A healthy, non-smoker, 58 year-old male patient presented for an evaluation of his posterior left mandible, which had a history of implant placement with recurrent periimplant infections. Significant clinical findings included several fistulous tracts and periodontal depth of 10 mm around implants. Radiographic examination was performed and revealed advanced periimplantitis with associated vertical bone loss.
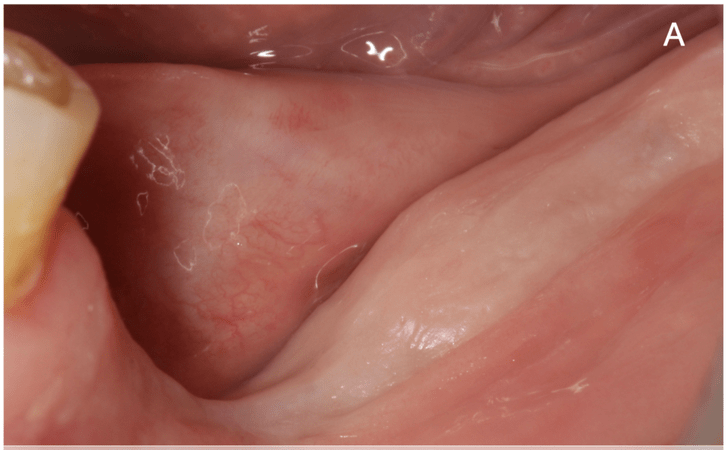
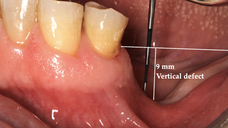
Second left mandibular molar extraction as well as implants explantation was performed because the prognosis was poor. Following a 2-months healing period, a severe vertical ridge defect (9 mm height) was noted as expected.
The vertical defect significantly compromised the site to implant placement. The patient desired a fixed rehabilitation; therefore, and after periodontal disease was controlled, the clinical plan was regenerate the alveolar defect tridimensional in order to ideally reconstruct form and function with a favourable implant-crown ratio and hygiene maintenance of the fixed prosthetic restoration.
Treatment Planning
Significant clinical findings included several fistulous tracts and periodontal depth of 10 mm around implants. Radiographic examination was performed and revealed advanced periimplantitis with associated vertical bone loss.
Progress & Completion
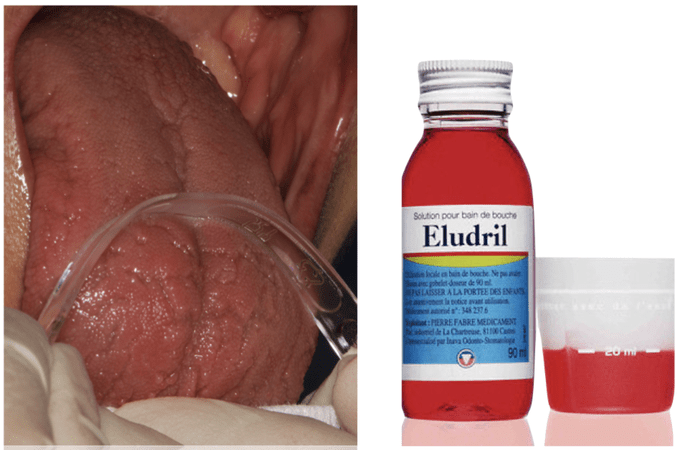
The patient was premedicated with amoxicillin 2 gr 1 hour before surgery and was given 1 gr penicillin 2 times a day for 1 week following surgery. The patient rinsed with 0.12% chlorhexidine solution (Eludril®) for 1 minute prior to surgery, and the tongue was scraped.
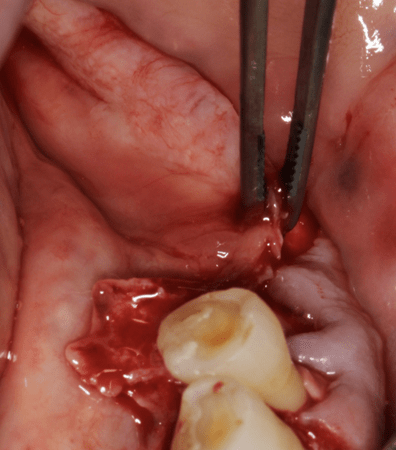
A full thickness, midcrestal incision was made in the keratinized gingiva on the alveolar crest, within 2 mm of the retromolar pad, and for adequate surgical access, a distal oblique vertical incision toward the coronoid mandibular process. A vertical incision was made mesiobuccally two teeth away and a 3-4 mm mini-incision is placed at the mesio-lingual line angle of the most distal tooth. The retromolar pad is gently elevated, lifted and incorporates a lingual flap.
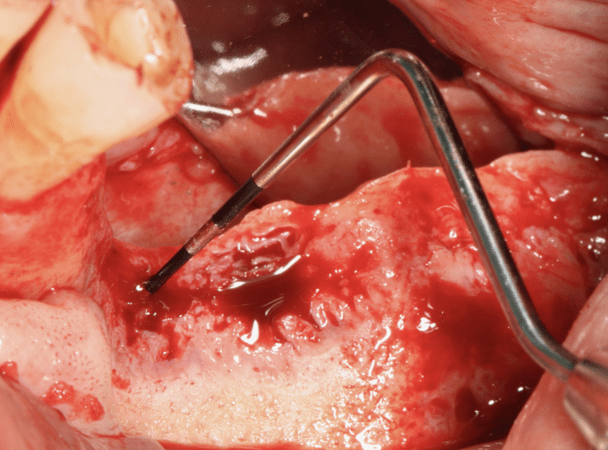
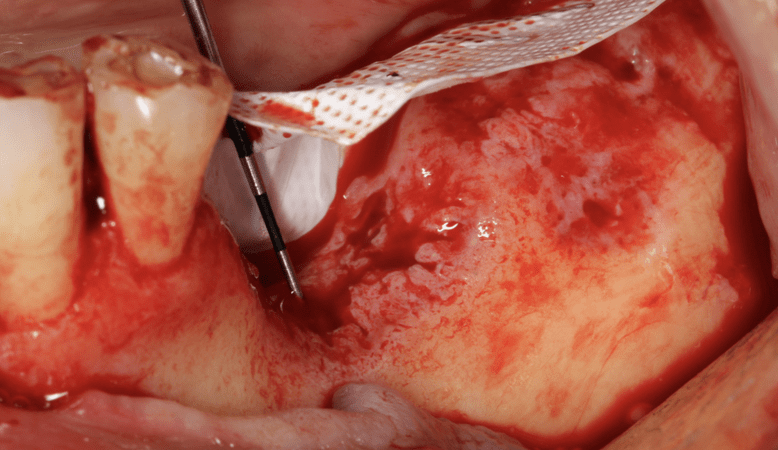
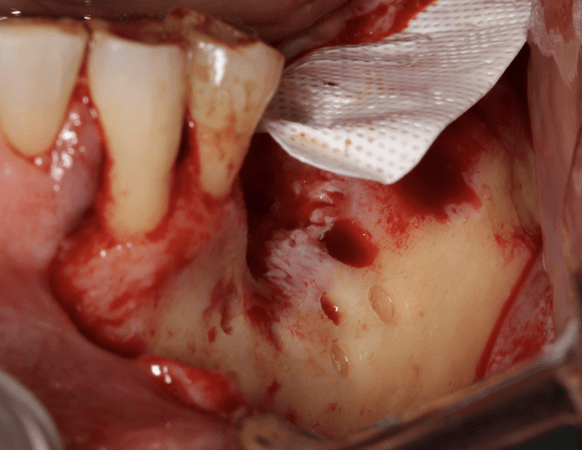
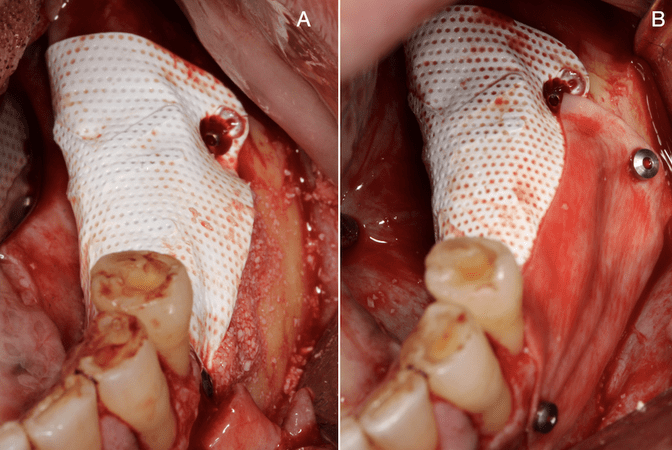
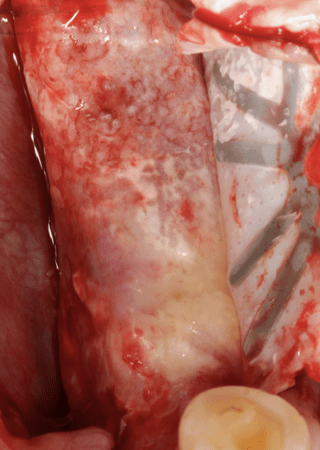
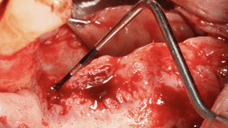
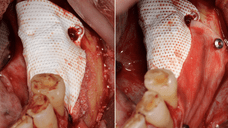
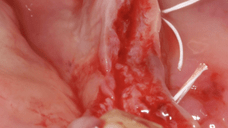
The lingual flap was elevated to the mylohyoid line (high mylohyoid line) and carefully separated from ascending fibers of mylohyoid muscle. The exposed bone was cleaned of all soft tissue remnants; An appropriately sized, titanium-reinforced dense polytetrafluoroethylene non-resorbable membrane (d-PTFE; Cytoplast® Ti-250, Osteogenics Biomedical, Inc., Lubbock, Texas) was selected and trimmed to completely cover the graft volume. With a small bur, the recipient bony bed was prepared with multiple decorticate holes to expose the medullary space.
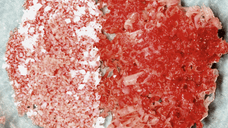
Autogenous bone was harvested from the left mandibular ascending ramus with safescraper twist curved®. The autogenous bone was mixed with ABBM (Bio-Oss®,Geistlich Pharma AG, Wolhusen, Switzerland).
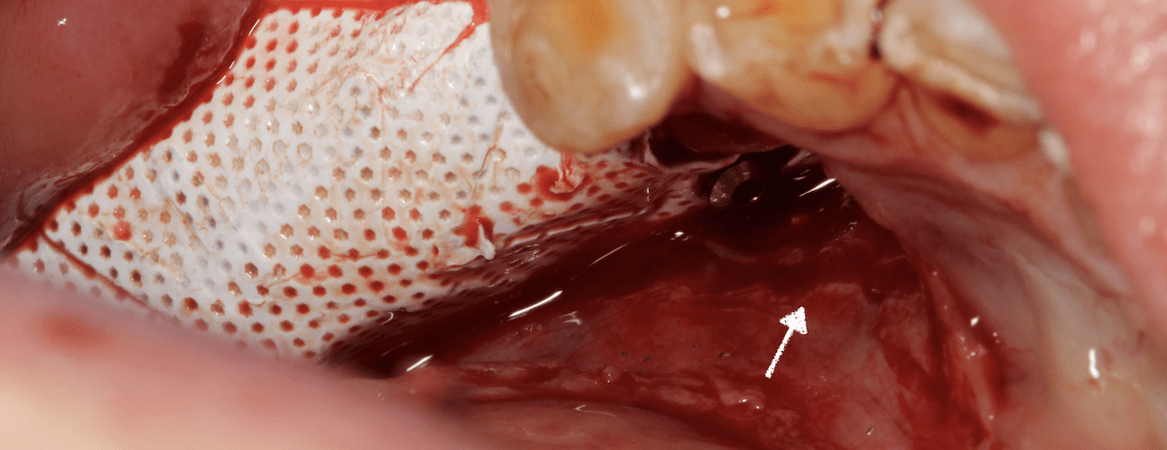
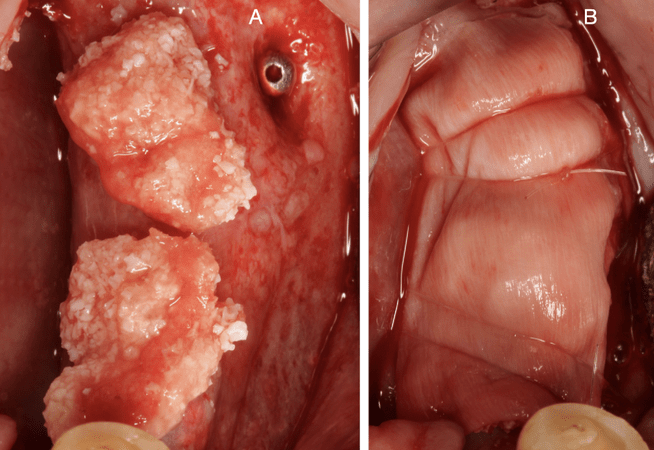
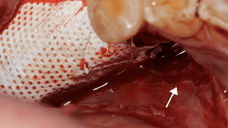
The membrane was fixated first on the lingual side using multiple pins (Master Pin control fixation®, Meisinger, Neuss, Germany). The autogenous particulate composite graft was placed appositionally on the vertical alveolar defect, and the membrane was folded over onto the buccal alveolus and fixated with additional titanium pins. The medial border was placed 3 mm from the distal surface of the first left premolar to prevent membrane exposure. A resorbable collagen membrane (Biogide®, Geistlich Pharma AG, Wolhusen, Switzerland) was applied to protect and contain the graft apically and minimize postoperative complications.
The lingual flap advancement at the “deep” mylohyoid attachment was made with a horizontal “hockey stick” periosteal incision with the blade tip sweeping through the periosteum. Advancement of all three zones of the lingual flap allows a completely relaxed lingual flap. Periosteal releasing incisions at the buccal flap were performed to provide adequate flap reflection for tension-free primary closure.
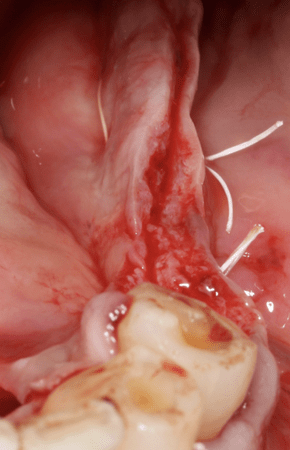
The flap was closed in two layers with the use of horizontal mattress (Cytoplast PTFE suture®, Osteogenics, 3- 0) and single interrupted sutures (Supramid®, B Braun Medical, 4-0). Medications were followed as described earlier. In addition, an anti-inflammatory medication, 600mg ibuprofen+arginate was prescribed two times a day for five days. For chemical plaque control, 0,12% chlorhexidine solution was used three times a day from 24 hours post-surgery until the time of suture removal. Postoperative swelling was significant, reaching maximum at 48 hours; swelling disappeared completely after twelve days. Discomfort was referred and was associated with tension from the swelling. Pain was minimal. No other symptoms occurred during post-surgical period. No removable appliance was used to avoid trauma.
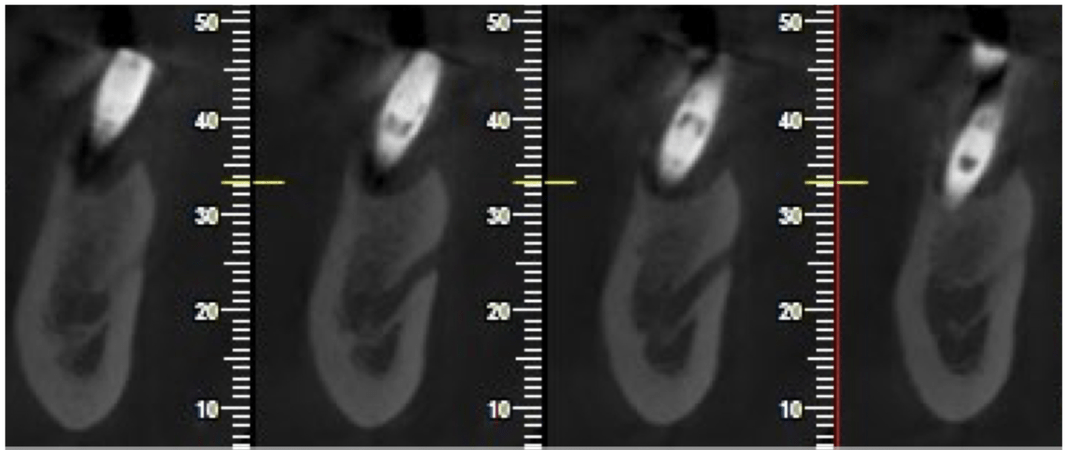
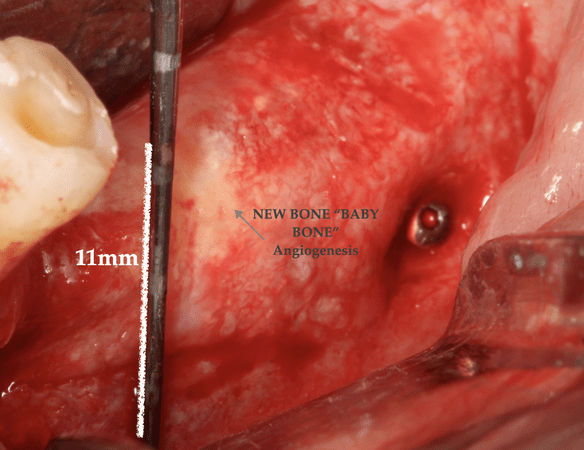
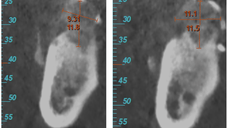
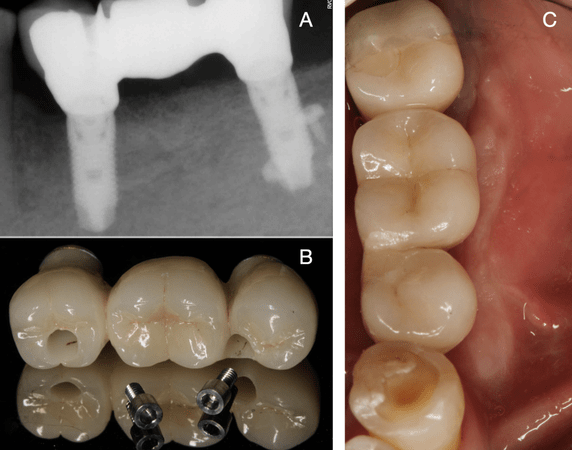
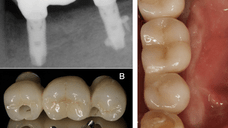
After nine months of uneventful healing, a radiographic examination (Cone Beam Computerized Tomography - CBCT) was performed revealing a vertical bone gain of 9.31 mm and 11.1 mm in premolar and molar left mandibular regions.
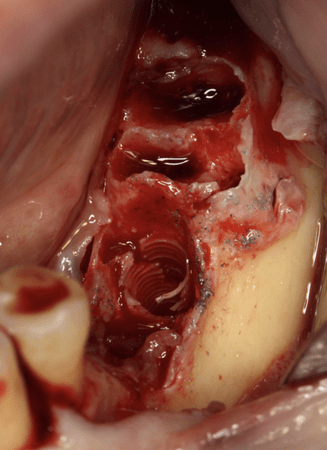
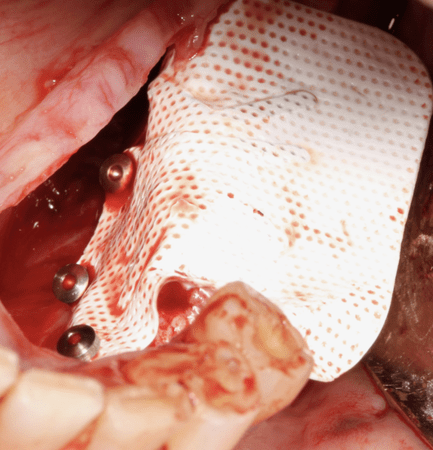
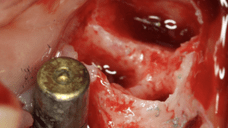
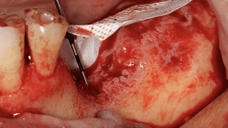
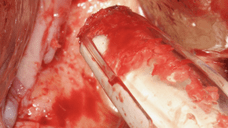
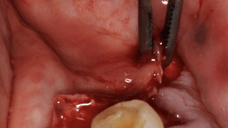
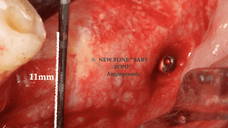
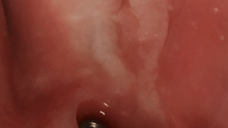
The area was opened using the same full-thickness flap design. The membrane had maintained its original position, and bone growth was evident. After the removal of the titanium pins and the d-PTFE, complete vertical bone regeneration was observed.
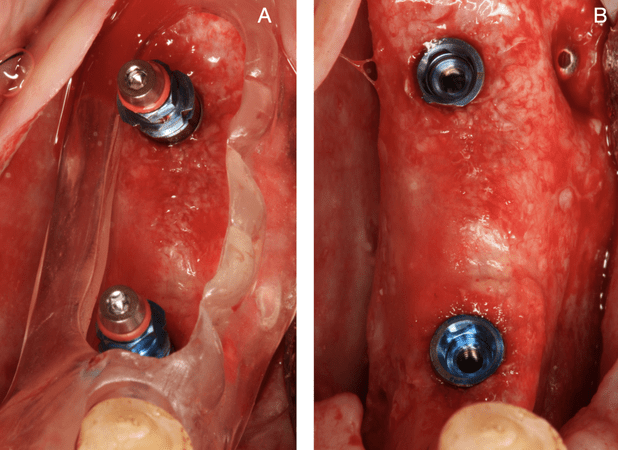
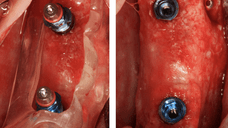
Two BTI Implants were placed (BTI®-Biotechnology Institute S.L., Vitoria, Spain) in accordance with the manufacturer’s protocol and with surgical guidance. After implant placement, a protective micro-sausage with 70% ABBM and 30% autogenous bone was placed on top of the implants over the newly formed crestal bone to protect the graft from possible early remodeling.
The implants were submerged through a 2-stage technique for 6 months. After 3.5 months, a soft tissue augmentation (free gingival graft-strip technique) was used to gain soft tissue volume and keratinized tissue. After 2.5 more months, the implants were uncovered and restored with a splinted three-unit implant supported fixed partial denture with no pink ceramic. The patient was entered into a scheduled maintenance program that included a clinical examination every six months and annual radiographic examination.
Follow-up & Outcome
Vertical ridge augmentation (VRA) is one of the greatest challenges for bone in implant therapy; it is biologically demanding, as angiogenesis must reach a certain distance from existing bone to new bone can be formed.
On the other hand, VRA is technique sensitive, and complications intra and post-operative can occur. However, in cases with limited bone availability for placing short implants, or due to restorative considerations, VRA offers the possibility to augment lost bony structures and improve aesthetic outcomes.
Long-term studies concluded that vertically augmented bone using GBR techniques responds to implant placement in a similar fashion to native bone; is safe and predictable, with minimal complications.